 Oct, 12 2025
Oct, 12 2025
When you need fast, reliable relief from joint pain, figuring out which drug fits your lifestyle can feel like a puzzle. Cobix is a brand name for celecoxib, a selective COX‑2 inhibitor used to treat arthritis and acute pain. It promises fewer stomach issues than traditional NSAIDs, but is it truly the best option for you? This guide breaks down Cobix side‑by‑side with its most common alternatives, so you can decide based on efficacy, safety, cost and convenience.
What is Cobix (Celecoxib)?
Celecoxib is a prescription non‑steroidal anti‑inflammatory drug (NSAID) that selectively blocks the COX‑2 enzyme. By sparing COX‑1, it reduces inflammation without compromising the protective lining of the stomach. Approved in 1999, celecoxib is listed on the WHO’s Essential Medicines list for osteoarthritis, rheumatoid arthritis and acute musculoskeletal pain. Typical dosages range from 100mg to 200mg daily, taken with food to improve absorption.
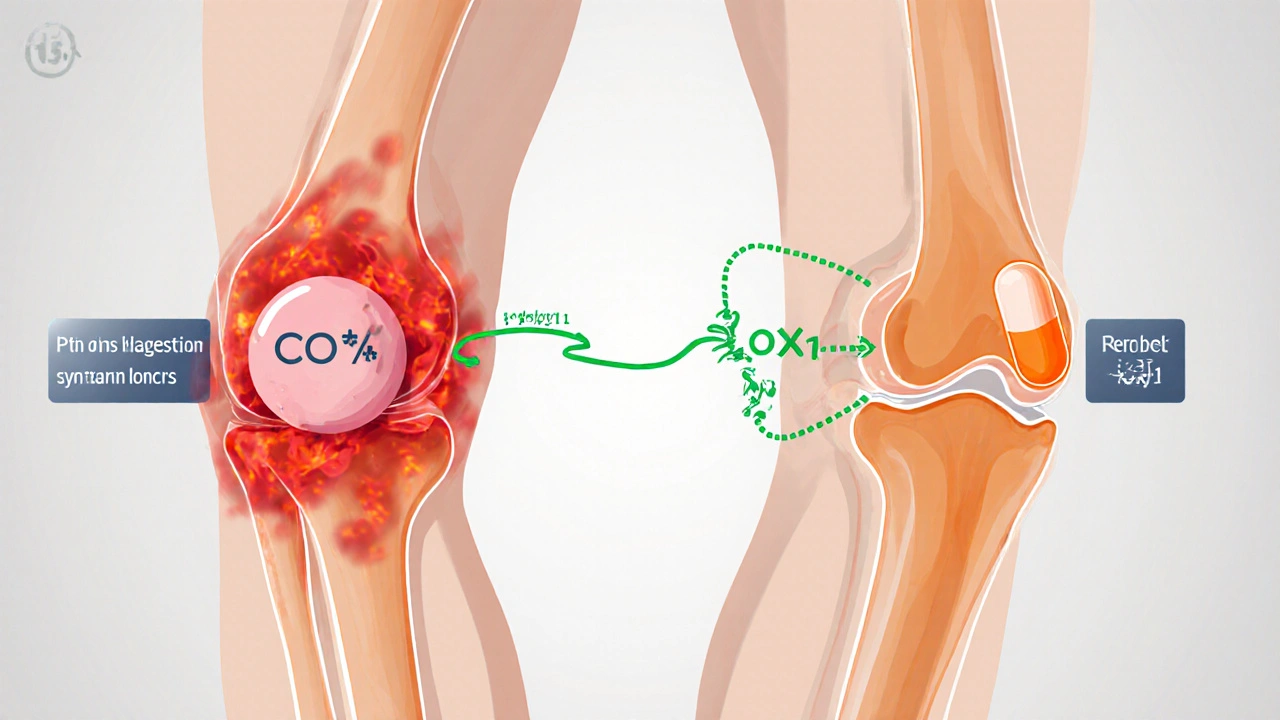
How does a COX‑2 inhibitor differ from traditional NSAIDs?
Traditional NSAIDs-think Ibuprofen and naproxen-block both COX‑1 and COX‑2 enzymes. COX‑1 helps protect the stomach lining and supports platelet function. When COX‑1 is inhibited, you’re more likely to experience gastric irritation, ulcers and increased bleeding risk. Cox-2 inhibitor celecoxib targets only the inflammation‑driving COX‑2, aiming for a cleaner safety profile, especially for adults with a history of GI problems.
Key alternatives to Cobix
Below are the most frequently prescribed or OTC alternatives you’ll encounter in a pharmacy or clinic.
- Ibuprofen - a short‑acting, non‑selective NSAID widely used for mild to moderate pain.
- Naproxen - a longer‑acting NSAID that stays in the system up to 12hours.
- Diclofenac - available as oral tablets, gels and patches; strong anti‑inflammatory power.
- Meloxicam - a semi‑selective COX‑2 inhibitor, often prescribed for chronic arthritis.
Side‑effect profile comparison
Understanding the safety trade‑offs is essential, especially if you’re managing other health conditions.
| Drug | Class | Typical Dose | Onset (hrs) | Common Side Effects |
|---|---|---|---|---|
| Cobix (Celecoxib) | Selective COX‑2 inhibitor | 100‑200mg daily | 1‑2 | Headache, mild GI upset, hypertension |
| Ibuprofen | Non‑selective NSAID | 200‑400mg q6‑8h | 0.5‑1 | Stomach pain, nausea, increased bleeding risk |
| Naproxen | Non‑selective NSAID | 250‑500mg bid | 1‑2 | GI irritation, dizziness, renal strain |
| Diclofenac | Non‑selective NSAID | 50‑75mg tds | 0.5‑1 | Liver enzyme elevation, CV risk, GI upset |
| Meloxicam | Semi‑selective COX‑2 inhibitor | 7.5‑15mg daily | 1‑2 | Mild GI issues, edema, headache |
Effectiveness for different conditions
All five drugs reduce inflammation, but their performance shifts depending on the condition.
- Osteoarthritis: Clinical trials show celecoxib (Cobix) provides comparable pain relief to naproxen while causing fewer GI complications.
- Rheumatoid arthritis: Both celecoxib and meloxicam are approved; meloxicam’s longer half‑life makes once‑daily dosing attractive for patients who struggle with adherence.
- Acute injury (sprains, strains): Ibuprofen and diclofenac act faster, making them popular for short‑term, high‑intensity pain.
- Post‑operative pain: Diclofenac patches deliver localized relief without systemic exposure, a niche where oral celecoxib isn’t as useful.
Cost considerations in 2025
Price can be a deciding factor, especially for long‑term therapy.
- Cobix (Celecoxib): Branded price averages $0.60 per 100mg tablet in the U.S.; generic celecoxib drops to $0.25 per tablet.
- Ibuprofen: OTC 200mg tablets cost about $0.03 each; bulk packs bring the cost below $0.01 per dose.
- Naproxen: OTC 250mg tablets run $0.04 each; prescription strength (500mg) costs $0.08.
- Diclofenac: Oral tablets $0.20 per 50mg; topical gels $15 per 30g tube (approx. 12 applications).
- Meloxicam: Generic oral 7.5mg costs $0.30 per tablet; the extended‑release version is $0.45.
If your insurance covers the brand, Cobix may be comparable to generic celecoxib. Otherwise, many patients opt for OTC ibuprofen for occasional flare‑ups due to its low price point.
Special populations and contraindications
Choosing a pain reliever isn’t just about the headline efficacy; you have to consider age, comorbidities and other meds.
- Elderly (≥65years): COX‑2 inhibitors like celecoxib reduce ulcer risk, but they carry a modest increase in cardiovascular (CV) events. Ibuprofen and naproxen also raise CV risk, but naproxen’s risk profile is slightly lower.
- Patients with hypertension: Celecoxib can elevate blood pressure; meloxicam and diclofenac have similar effects. Avoid high‑dose NSAIDs if BP is uncontrolled.
- Kidney disease: Non‑selective NSAIDs (ibuprofen, naproxen, diclofenac) have stronger nephrotoxic potential. Celecoxib and meloxicam are gentler but still require monitoring.
- Pregnancy: All NSAIDs are discouraged after 20weeks gestation. Diclofenac patches may be used under strict supervision for early‑term back pain, but generally, acetaminophen is preferred.
- History of ulcers: Celecoxib and meloxicam are safer choices; however, adding a proton‑pump inhibitor (PPI) can mitigate risk for any NSAID.
Practical tips for switching or combining therapy
Doctors sometimes rotate between drugs to chase the best pain control while limiting side effects.
- Start with the lowest effective dose of a single agent. For most adults, ibuprofen 200mg q6h works for mild flare‑ups.
- If GI upset appears, switch to celecoxib 100mg daily and add a PPI such as omeprazole 20mg.
- For chronic arthritis, consider meloxicam 7.5mg once daily; its long half‑life reduces pill burden.
- Avoid concurrent use of two NSAIDs; overlapping COX inhibition raises bleeding risk without added benefit.
- If you need breakthrough pain, a single dose of diclofenac gel (1‑2g) can be applied locally while continuing oral celecoxib.
Bottom line: When to choose Cobix
If you have a history of stomach ulcers, need daily arthritis control and can manage a modest increase in blood pressure, Cobix (celecoxib) offers a balanced mix of effectiveness and GI safety. For occasional aches, the cheaper OTC ibuprofen or naproxen usually suffice. When CV risk looms, naproxen remains the NSAID with the most favorable heart profile, while diclofenac should be reserved for short‑term, targeted use. Meloxicam sits in the middle-more selective than ibuprofen but less expensive than the branded COX‑2 inhibitors.
Frequently Asked Questions
Is Cobix safe for long‑term use?
Long‑term celecoxib can be safe if you have regular check‑ups for blood pressure, kidney function and cardiovascular health. Adding a low‑dose PPI helps protect the stomach. Always follow your doctor’s monitoring schedule.
Can I take Ibuprofen and Cobix together?
Combining two NSAIDs is not recommended. They increase the risk of stomach bleeding and kidney problems without providing extra pain relief. Choose one agent and stick with it, or talk to your physician about rotating therapies with a wash‑out period.
Which drug works fastest for a sudden back spasm?
Diclofenac gel or oral ibuprofen usually give the quickest onset (within 30‑60 minutes). If you need rapid relief and have no GI issues, a single 400mg ibuprofen dose is a common first step.
Is meloxicam a true COX‑2 inhibitor?
Meloxicam is semi‑selective: it prefers COX‑2 at low doses but can inhibit COX‑1 when taken higher. This gives it a safety profile between celecoxib and traditional NSAIDs.
How do insurance plans usually cover these drugs?
Most U.S. plans label celecoxib as a Tier3 or specialty drug, requiring prior authorization. Generic ibuprofen and naproxen are Tier1, meaning lower co‑pays. Check your formulary for exact tiers and any step‑therapy requirements.
Amy Carpenetti
October 12, 2025 AT 04:40Thanks for the rundown it really helps when you’re juggling meds and a budget. I appreciate the clear tabs on side‑effects and cost. I’ll chat with my doc about trying celecoxib if my stomach stays sensitive.
Paul Griffin
October 21, 2025 AT 10:53Excellent summary of the therapeutic landscape. The comparison of gastrointestinal risk versus cardiovascular considerations is particularly useful for clinicians. Your table format makes the data easily digestible. It would be beneficial to include a brief note on renal monitoring protocols for each agent. Overall a very practical resource for prescribing decisions.
Michael Tekely
October 30, 2025 AT 16:06Yo the COX‑2 vs non‑selective NSAID trade‑off is the classic pharmacodynamics showdown. If you’re chasing rapid onset you’ll gravitate to ibuprofen or diclofenac gel, but the GI‑sparing profile of celecoxib is a win for ulcer‑prone peeps. Remember that dose‑response curves aren’t linear – titrate to the lowest effective dose. Also, keep an eye on that systolic pressure when you go long‑term on Cobix.
Oscar Taveras
November 8, 2025 AT 22:20Thank you for assembling such a comprehensive guide. It is reassuring to see that there are viable options for patients with varying risk profiles. The emphasis on individualized therapy aligns well with patient‑centered care. I look forward to seeing more comparative studies that further clarify these choices.
katie clark
November 18, 2025 AT 04:33The exposition provides a commendably exhaustive enumeration of NSAID pharmacotherapy. Nonetheless, the discourse marginally neglects the nuanced pharmacokinetic disparities inherent to each molecule. A more erudite exploration of enzymatic selectivity could elevate the manuscript.
Victoria Guldenstern
November 27, 2025 AT 10:46It is truly astonishing how a simple table can encapsulate the entire saga of modern analgesia while simultaneously reminding us of the boundless ingenuity of pharmaceutical marketing campaigns that insist we believe a tiny chemical tweak can magically absolve us of all adverse effects however the data plainly reveal that each drug carries its own constellation of trade‑offs yet the narrative persists that celecoxib is the benevolent saviour for the ulcer‑prone patient while the rest of the class remains the villainous rogues in a melodramatic plot twist however one must acknowledge that the financial calculus wielded by insurers often dictates the ultimate choice more than any nuanced pharmacological superiority moreover the occasional mention of cardiovascular risk feels like an afterthought tossed in to satisfy regulatory checklists while the real concern for many remains the relentless rise in out‑of‑pocket expenses for the average consumer nevertheless patients do appreciate the convenience of once‑daily dosing even if it merely masks the underlying complexity of chronic inflammation management in truth the so‑called “semi‑selective” agents occupy a gray area that defies simple categorisation and invites endless debate over whether they truly bridge the gap between efficacy and safety or simply occupy a marketing niche that thrives on ambiguity finally the table’s clean layout offers a fleeting moment of clarity in a sea of medical jargon that otherwise threatens to drown the layperson in a deluge of statistics and footnotes
Bill Bolmeier
December 6, 2025 AT 17:00Michael you nailed the science but don’t forget the human side ‑ patients are scared of pills and love a clear plan – so keep it simple and push the celecoxib option when the stomach’s at risk!
Tom Smith
December 15, 2025 AT 23:13Of course because simplifying complex pharmacology always ends well.
Kyah Chan
December 25, 2025 AT 05:26The preceding analysis, while thorough, fails to address the systemic biases introduced by pharmaceutical sponsorship which undeniably skew clinical practice guidelines toward newer, profit‑driven agents such as celecoxib; consequently, a more critical appraisal of the underlying evidence base is warranted to safeguard patient autonomy and public health integrity.
Ira Andani Agustianingrum
January 3, 2026 AT 11:40Great job breaking all that down! If you’re new to this, start with the cheapest over‑the‑counter option and see how you feel. Switch to a prescription COX‑2 only if you notice stomach trouble. Keep an eye on your blood pressure and stay in touch with your doctor.
James Higdon
January 12, 2026 AT 17:53It is morally indefensible to prescribe any medication without fully considering the long‑term societal costs associated with increased cardiovascular events, and thus clinicians have an ethical duty to prioritize agents with a proven safety record over newer, marketed alternatives.
Wanda Smith
January 22, 2026 AT 00:06The real story behind these drug comparisons is hidden in the data farms where algorithms decide which study gets funding and which narrative fits the agenda of shadowy health conglomerates; trust no one and read between the lines.