 Dec, 1 2025
Dec, 1 2025
Anticholinergic Burden Calculator
Most people reach for diphenhydramine (Benadryl) when they have allergies, a runny nose, or trouble sleeping. It’s cheap, easy to find, and works fast. But what most users don’t realize is that every time they take it, they’re not just blocking histamine-they’re flooding their brain with a drug that shuts down key functions needed to stay alert, focused, and safe. First-generation antihistamines like diphenhydramine, chlorpheniramine, and promethazine are not harmless sleep aids. They’re powerful CNS depressants with side effects that can last longer than you think-and carry real risks, especially for older adults and drivers.
How These Drugs Work (And Why They Make You Sleepy)
First-generation antihistamines were developed in the 1940s to block histamine, the chemical your body releases during allergic reactions. But unlike newer versions, they don’t stop at the site of the allergy. Their small, oily molecules slip easily through the blood-brain barrier. Once inside the brain, they bind tightly to H1 receptors, which normally help keep you awake and alert. By turning these receptors off, they cause intense drowsiness.
It’s not just histamine they block. These drugs also strongly attach to muscarinic receptors-the same ones targeted by drugs used to treat overactive bladder or Parkinson’s. That’s why you get dry mouth, blurred vision, trouble urinating, and constipation. These are classic anticholinergic effects. Studies show that at standard doses, first-gen antihistamines occupy 30-50% of brain H1 receptors. Compare that to second-generation drugs like loratadine or cetirizine, which barely touch 5%. That’s why one makes you sleepy, and the other doesn’t.
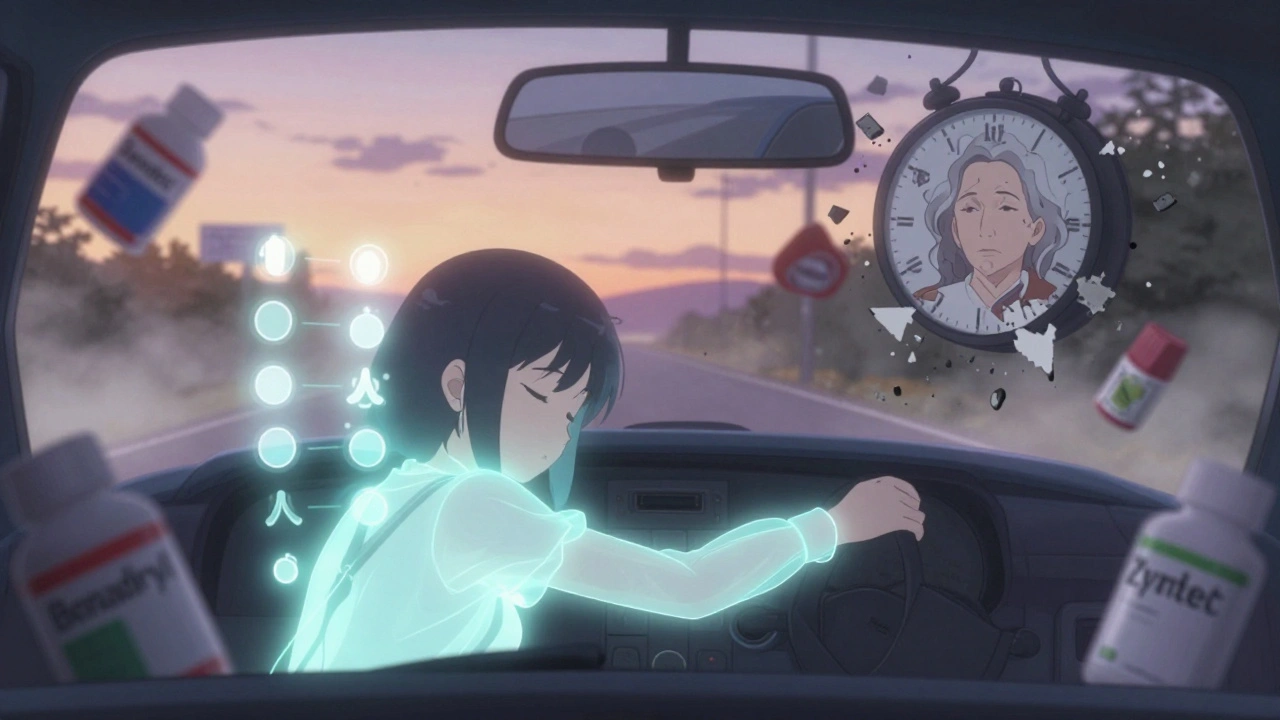
Brain concentrations of diphenhydramine can hit 15-25 ng/mL within two hours of a 50 mg dose. That’s enough to slow reaction times, blur thinking, and make driving dangerous. Driving simulator studies show impairment levels as high as 0.8 out of 1.0-nearly as bad as being over the legal alcohol limit. And the effects don’t vanish when you wake up. Many people report a “hangover” feeling that lasts up to 18 hours after taking it.
The Real-World Impact: More Than Just Feeling Tired
If you’ve ever taken Benadryl for allergies and then felt too foggy to work, drive, or even hold a conversation, you’re not alone. On Drugs.com, 38% of users report “extreme sleepiness,” and 22% say they couldn’t concentrate. Reddit threads are full of stories like this one: “Took Benadryl at 8 PM for hives and woke up at 2 PM the next day feeling like I’d been hit by a truck.”
But the danger isn’t just about feeling sluggish. Emergency departments see a steady stream of cases linked to these drugs. In 2021, 35% of drowsy driving crashes involving medication were tied to first-generation antihistamines, according to NHTSA data. People don’t realize how long the effects last. They take it at night, feel fine in the morning, and get behind the wheel-only to find their reaction time is still slowed.
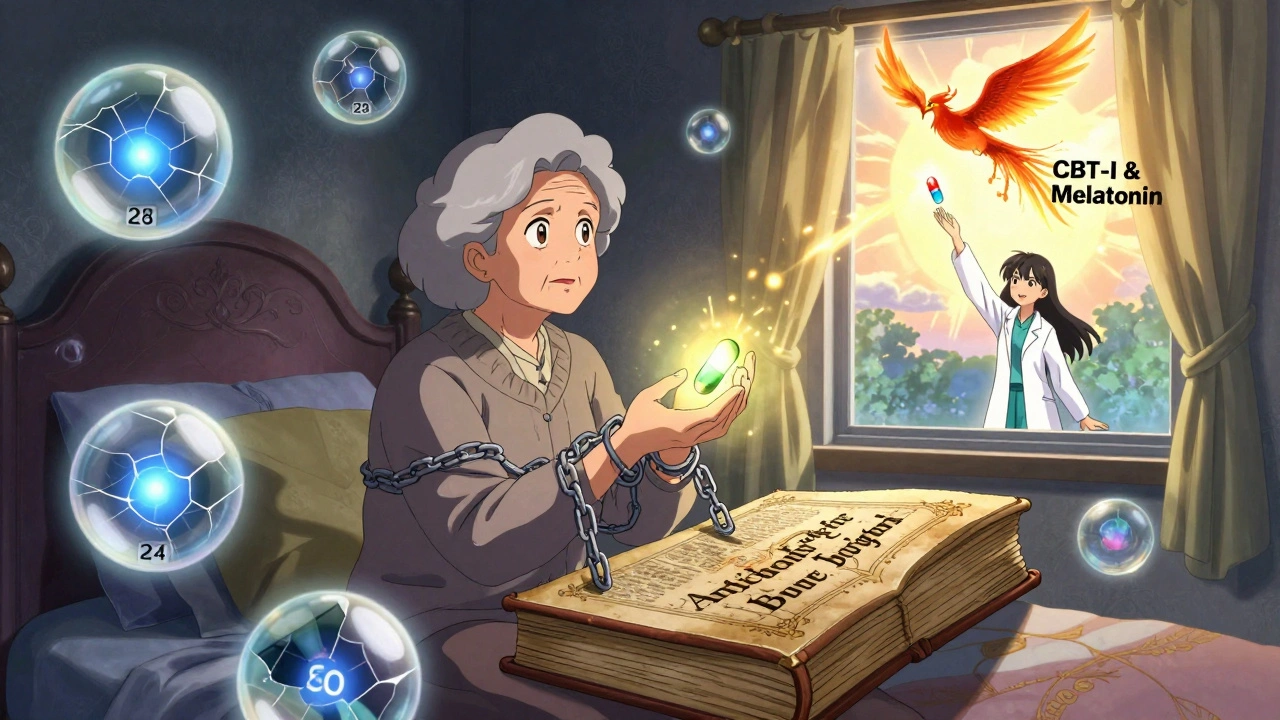
For older adults, the risks are even worse. The American Geriatrics Society lists diphenhydramine and similar drugs as “potentially inappropriate” for people over 65. Why? Because long-term use is linked to a 54% higher risk of cognitive decline and dementia. The anticholinergic burden adds up. Even low doses taken nightly for insomnia can lead to memory problems, confusion, and falls. A 2022 survey of 1,204 older adults found that while 65% said it helped them sleep, 42% struggled with morning confusion lasting three to four hours.
Why Do People Still Use Them?
If they’re so risky, why are they still on every pharmacy shelf?
Three reasons: cost, availability, and extra uses.
A bottle of 24 diphenhydramine tablets costs about $5. The same number of cetirizine tablets? Around $15. For people without insurance or on tight budgets, the price difference is hard to ignore.
They’re also sold over-the-counter with minimal warnings. While FDA labels include strong cautions about drowsiness, the small print on store shelves often downplays the danger. A 2022 JAMA Internal Medicine study found 45% of users underestimated how long the effects lasted.
And yes-they work well for things other than allergies. First-gen antihistamines are still the best option for motion sickness. They reduce nausea in 70-80% of users, compared to 40-50% for newer drugs. They’re also the most reliable short-term sleep aid, cutting sleep onset time by 30-40 minutes. For occasional use-say, a long car ride or one bad night of insomnia-they can still be useful.
But here’s the catch: if you’re using them regularly, you’re trading short-term relief for long-term risk.
Who Should Avoid Them Completely?
These drugs aren’t safe for everyone. Avoid them if you:
- Are over 65
- Have glaucoma, an enlarged prostate, or urinary retention
- Take other anticholinergic drugs (like some antidepressants, bladder meds, or Parkinson’s treatments)
- Drive, operate machinery, or work in safety-critical jobs
- Have liver disease (they’re broken down by CYP2D6 and CYP3A4 enzymes-poor metabolizers get much stronger effects)
- Drink alcohol (it increases brain penetration by 40-60%)
Even if you’re young and healthy, using them daily for months or years increases your anticholinergic load. That’s not something you can reverse by switching to a different pill tomorrow.
What Are the Alternatives?
Second-generation antihistamines-cetirizine (Zyrtec), loratadine (Claritin), fexofenadine (Allegra), and desloratadine (Clarinex)-are the clear first choice for most allergy sufferers. They don’t cross the blood-brain barrier significantly. Their sedation index is 0.1-0.3, compared to 0.7-0.9 for first-gen drugs. They last 12-24 hours, so you take them once a day. And they’re now widely available as generics, bringing the price gap down.
For sleep, melatonin or cognitive behavioral therapy for insomnia (CBT-I) are safer long-term options. For motion sickness, ginger supplements or scopolamine patches are more targeted and less sedating. For nausea, ondansetron (Zofran) works better without the brain fog.
And yes-there are even new drugs coming. Two candidates in Phase II trials (EB-029 and DP-118) are designed to block histamine in the body but barely enter the brain. Early results show 80% less CNS penetration while keeping the same allergy-fighting power. These could be the next generation of antihistamines-without the drowsiness.
How to Use Them Safely (If You Must)
If your doctor recommends a first-generation antihistamine for a specific reason-like motion sickness or short-term insomnia-follow these rules:
- Take it only at night. Never use it during the day unless you’re fully rested and won’t be driving or working.
- Start with the lowest dose possible. For diphenhydramine, that’s 12.5 mg, not 25 or 50.
- Wait at least 8 hours before driving or operating machinery. Even if you feel fine, your brain is still affected.
- Avoid alcohol completely. It makes the drowsiness worse and increases the risk of overdose.
- Don’t use it for more than a few days in a row. Chronic use increases dementia risk.
- Check all other meds you take. Many antidepressants, stomach meds, and pain relievers also have anticholinergic effects. Adding them together can be dangerous.
And if you’re taking one of these drugs every night for sleep? Talk to your doctor. There are better, safer ways to manage insomnia without risking your brain health.
What’s Changing? Regulations and Awareness
Regulators are catching up. The UK banned over-the-counter sales of promethazine to minors in 2022. The FDA is reviewing similar restrictions on diphenhydramine after pediatric ER visits rose 27% between 2018 and 2022. In 2022, the FDA issued new draft guidelines requiring stronger labeling about next-day impairment.
Pharmacies are starting to put warning stickers on shelves. Some are moving these drugs behind the counter. The American College of Allergy, Asthma, and Immunology now says first-gen antihistamines should be “reserved for short-term use in specific indications”-not daily allergy relief.
Market analysts predict a 15-20% drop in OTC sales by 2030 as cheaper, safer alternatives become more common. But until then, the choice is yours.
Just know this: every time you take a first-generation antihistamine, you’re not just treating an allergy. You’re temporarily shutting down parts of your brain. And if you do it often enough, the damage might not be temporary at all.
Jay Everett
December 2, 2025 AT 18:50Bro, I took Benadryl last week for a rash and woke up at 3 PM feeling like my brain had been replaced with wet sand 🤯. I tried to make coffee and spilled it everywhere. Then I stared at the toaster for 10 minutes wondering why it wasn't working. Turns out my frontal lobe was on vacation. First-gen antihistamines are basically brain fog in a pill. Don't be that guy who thinks 'it's just sleep aid' - it's a chemical lobotomy with a side of dry mouth.
मनोज कुमार
December 4, 2025 AT 06:17Anticholinergic burden is a real pharmacokinetic concern especially in polypharmacy elderly populations. H1 receptor occupancy >30% correlates with cognitive impairment metrics. OTC availability is a regulatory failure. End.
dave nevogt
December 5, 2025 AT 10:34It’s funny how we treat our brains like they’re just another organ we can temporarily disable without consequence. We’ll pop a pill for a sneeze and call it harmless, but we’d never think to pour a shot of whiskey into our coffee and call it a ‘natural energy boost.’ The truth is, we’ve normalized chemical sedation because it’s cheap, convenient, and marketed as ‘just a little help.’ But what we’re really doing is trading moments of comfort for decades of mental erosion - and we don’t even notice until we forget our kid’s name or get lost driving home from the grocery store. It’s not just drowsiness. It’s slow-motion dementia, packaged as allergy relief.
Steve World Shopping
December 7, 2025 AT 06:39You're all missing the point. These drugs are not the problem. The problem is the population that takes them without understanding pharmacodynamics. You want to blame the pill? Blame the person who thinks 'it's just a sleep aid' while taking it with Zoloft, gabapentin, and a beer. Anticholinergic load isn't about the drug - it's about the idiot stacking them like Legos. Wake up.
Lynn Steiner
December 7, 2025 AT 10:30I used to take Benadryl every night for years. I thought it was helping me sleep. Turns out it was just slowly erasing my memories. I forgot my wedding anniversary. I forgot my dog's name. I forgot I had a kid. Now I cry every time I see a bottle. I'm not okay. 🥺
Alicia Marks
December 8, 2025 AT 14:54Switched to Zyrtec last year. No more 12-hour fog. No more morning confusion. My brain came back. You don’t need to suffer to sleep better. There are safer ways. 💪
Steve Enck
December 9, 2025 AT 05:43It is imperative to recognize that the normalization of first-generation antihistamine usage represents a profound epistemological failure in public health literacy. The commodification of sedation as a therapeutic intervention, coupled with the absence of mandatory cognitive risk disclosures on packaging, constitutes a systemic violation of the principle of informed consent. One cannot ethically justify the widespread dissemination of a pharmacological agent that demonstrably impairs executive function, particularly when safer alternatives are both accessible and affordable. This is not a matter of personal preference - it is a public health catastrophe in slow motion.
Joel Deang
December 10, 2025 AT 08:10so i took benadryl last night for my allergies and woke up at 1pm feeling like i got hit by a truck 😅 and then i tried to text my boss and i sent him ‘im sry i cant come in today i think my brain is on vaction’ and he replied ‘u good bro?’ lol i think i’m gonna switch to allegra. no more brain fog for me 🙃
Roger Leiton
December 10, 2025 AT 08:24Just did a deep dive on this after reading the post - and holy smokes, I had no idea. I’ve been using diphenhydramine for years as a sleep aid. I thought I was being smart by taking it at night. Turns out I’ve been slowly turning my brain into Swiss cheese 🧀. I just ordered Zyrtec and melatonin. Time to give my hippocampus a break. Thanks for the wake-up call! 🙏
Laura Baur
December 11, 2025 AT 13:53It's not just about the drugs - it's about the culture that allows them to be sold like candy. You walk into any pharmacy and there they are, right next to the gum and the batteries, with no warning bigger than a tiny font that says 'may cause drowsiness.' Meanwhile, a bottle of ibuprofen has a 12-point warning label about gastrointestinal bleeding. Why? Because people are dying from anticholinergic toxicity, and nobody in charge wants to admit that the system is broken. We treat our brains like disposable batteries, and then we wonder why dementia rates are skyrocketing. This isn't just bad medicine - it's moral negligence.
Jack Dao
December 13, 2025 AT 06:44Wow. You people are so dramatic. It’s a pill. People have been using this for 70 years. If you’re too lazy to read the label, don’t blame the drug. My grandpa took Benadryl every night for 40 years and lived to 92. He was sharp as a tack until the day he died. You think science is going to stop because you’re too weak to handle a little drowsiness? Grow up.
Paul Keller
December 15, 2025 AT 04:38Look, I get it - the science is solid. But for people who can’t afford $15/month for Zyrtec, or who have no access to CBT-I, these drugs are a lifeline. The real issue isn’t the pill - it’s the healthcare system that leaves people with no real alternatives. We need better access, not more guilt trips. I’m not saying use them daily - but don’t shame the person who takes one to get through a night of insomnia because they can’t afford therapy or can’t find a doctor. Compassion over condemnation.
Shannara Jenkins
December 16, 2025 AT 20:05My mom used to take Benadryl for sleep. Last year she fell and broke her hip - the ER doc said it was likely because of the anticholinergic effects. She switched to melatonin and now she’s hiking again. Don’t wait until it’s too late. Your brain deserves better. ❤️
Elizabeth Grace
December 17, 2025 AT 21:18I used to love Benadryl. Now I hate it. I took it for a week during a bad allergy flare and felt like I was underwater for days. My husband said I kept asking the same questions over and over. I didn’t even realize I was being weird. That’s when I knew - it’s not just sleep. It’s brain rot. I’m done.
Arun kumar
December 18, 2025 AT 00:30in india we call it cromal or diphenhydramine and everyone uses it for sleep and allergies. no one knows about the long term risks. i just told my uncle who takes it every night - he said 'but it works' 😅 we need more awareness here too