 Oct, 14 2025
Oct, 14 2025
OCD and SAD Symptom Tracker
Daily Tracking
Tracking History
| Date | Mood | Compulsion | Daylight | Seasonal Impact |
|---|
Pattern Analysis
Seasonal Management Tips
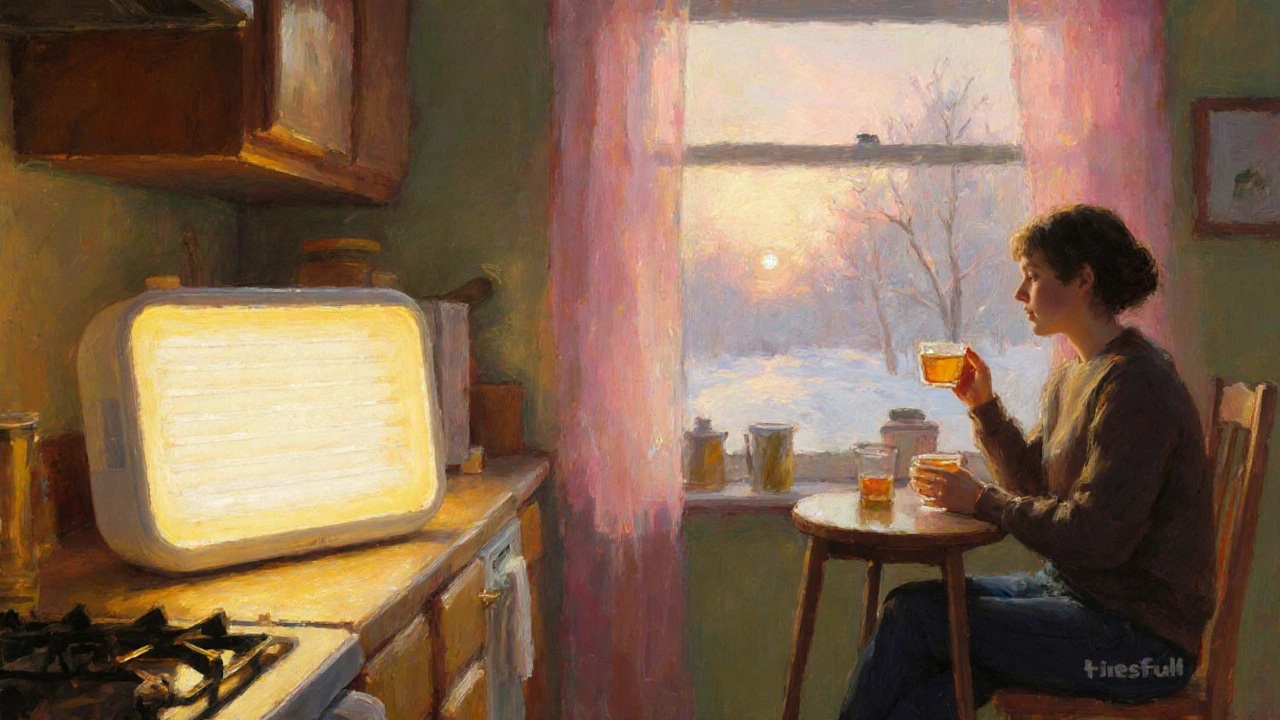
Try a 15-minute morning light session using a light box or natural window light. This can lift serotonin levels and reduce compulsions before the day starts.
Allocate 15 minutes daily to write down intrusive thoughts. Afterward, deliberately postpone compulsive actions until after this time slot.
Regular aerobic activity like brisk walking can boost endorphins and help reset your circadian rhythm, reducing both depressive and obsessive symptoms.
Ever wondered why some people notice a spike in their compulsive rituals when the days get shorter? That link isn’t a coincidence - there’s a real OCD and SAD connection worth understanding. In this guide we’ll break down what each condition looks like, why they sometimes walk hand‑in‑hand, and what you can do if you or a loved one are dealing with both.
What Is Obsessive‑Compulsive Disorder?
Obsessive‑Compulsive Disorder is a chronic mental‑health condition characterized by intrusive thoughts (obsessions) and repetitive behaviors (compulsions) aimed at reducing anxiety. In the UK, about 1.2% of adults meet diagnostic criteria, with onset often in late teens or early twenties.
Key attributes:
- Common obsessions: contamination, symmetry, aggressive urges.
- Typical compulsions: washing, checking, ordering.
- Neurobiology: dysregulated serotonin and glutamate pathways.
- Treatment mainstays: cognitive‑behavioural therapy (CBT) with exposure‑response prevention, selective serotonin reuptake inhibitors (SSRIs).
What Is Seasonal Affective Disorder?
Seasonal Affective Disorder (SAD) is a subtype of major depressive disorder that recurs seasonally, most often in the autumn and winter months when daylight hours shrink. Roughly 5% of the UK population experiences clinically significant SAD, with higher rates at higher latitudes.
Core features:
- Low mood, loss of interest, fatigue.
- Increased appetite (especially carbs) and weight gain.
- Hypersomnia or oversleeping.
- Biological triggers: reduced melatonin, altered circadian rhythms, serotonin dips.
- First‑line treatment: bright‑light therapy, CBT‑SAD, occasional SSRIs.
Why Do OCD and SAD Often Appear Together?
Researchers have identified several overlapping mechanisms that help explain the comorbidity:
- Serotonin dysfunction. Both disorders show decreased serotonergic activity, which is why SSRIs can improve symptoms in OCD and SAD alike.
- Circadian rhythm disruption. Shorter daylight interferes with sleep‑wake cycles, heightening anxiety that fuels compulsions.
- Genetic predisposition. Twin studies reveal shared heritability estimates of roughly 30% for both conditions.
- Stress‑reactive coping. Seasonal stress (e.g., feeling isolated during winter) may trigger obsessive checking or cleaning as a maladaptive coping tool.
These shared pathways mean that when one condition flares, the other is more likely to follow.
How the Symptoms Overlap
| Feature | Obsessive‑Compulsive Disorder | Seasonal Affective Disorder |
|---|---|---|
| Primary Mood | Anxiety‑driven distress | Low‑energy depression |
| Sleep Changes | Insomnia from intrusive thoughts | Hypersomnia or early‑morning awakening |
| Appetite | Often unchanged; some may over‑eat to self‑soothe | Increased carbohydrate cravings, weight gain |
| Energy Levels | Fluctuating; compulsions can be exhausting | General fatigue, sluggishness |
| Response to Light | Light exposure can lower anxiety, but not a primary treatment | Bright‑light therapy is a cornerstone |
Diagnosing Co‑Occurring OCD and SAD
Clinicians follow a two‑step assessment:
- Screen for each disorder separately using validated tools - the Yale‑Brown Obsessive‑Compulsive Scale (Y‑BOCS) for OCD and the Seasonal Pattern Assessment Questionnaire (SPAQ) for SAD.
- Evaluate timing and severity. If depressive episodes align with reduced daylight and compulsions intensify during those months, a comorbid diagnosis is likely.
It’s crucial to rule out other mood or anxiety disorders that can masquerade as either condition.
Treatment Strategies When Both Conditions Co‑Exist
Because the disorders share serotonin pathways, many treatment plans blend approaches.
- Medication. An SSRI such as sertraline or fluoxetine often addresses both OCD obsessions and SAD‑related low mood. Dose adjustments may be needed during winter months.
- Bright‑Light Therapy. A 10,000‑lux light box used for 30‑45 minutes each morning can synchronize circadian rhythms, indirectly reducing anxiety that fuels compulsions.
- CBT with Exposure‑Response Prevention (ERP). Tailor ERP to include seasonal triggers - for example, gradually reduce checking behaviours that spike during dark evenings.
- Sleep Hygiene. Consistent bedtime, limiting screen exposure after dark, and using a dawn simulator can blunt both depressive and obsessive cycles.
- Lifestyle Adjustments. Regular outdoor activity, vitamin D supplementation (particularly in the UK), and balanced nutrition help stabilise mood and anxiety.
Therapists often schedule more frequent sessions in the autumn to pre‑empt winter flare‑ups.
Practical Tips for Managing Daily Life
If you’re juggling OCD and SAD, these day‑to‑day habits can make a big difference:
- Morning Light Routine. Sit by a window or use a light box while having breakfast. Even 15 minutes can lift serotonin.
- Schedule “Worry Windows”. Allocate a brief, timed slot each day to write down intrusive thoughts, then deliberately postpone compulsive actions until after the slot.
- Exercise. Moderate aerobic activity (e.g., brisk walking) boosts endorphins and helps reset circadian timing.
- Social Support. Share your seasonal pattern with friends or support groups; accountability reduces isolation.
- Track Mood & Behavior. Use a simple spreadsheet or phone app to log daylight exposure, mood rating (1‑10), and compulsive urge intensity. Patterns become easier to spot.
When to Seek Professional Help
Contact a mental‑health professional if you notice any of the following:
- Compulsions that take more than an hour each day. \n
- Depressive symptoms that last longer than two weeks or severely impair work/social life.
- Thoughts of self‑harm or hopelessness.
- Failure of self‑management strategies after a month of consistent effort.
Early intervention can prevent a winter‑time spiral where OCD and depression reinforce each other.
Key Takeaways
- OCD and SAD share serotonin dysfunction, circadian disruptions, and genetic risk factors.
- Symptoms often overlap - insomnia, fatigue, and heightened anxiety are common during darker months.
- Combined treatment (SSRIs, bright‑light therapy, CBT‑ERP) works better than tackling each disorder separately.
- Simple lifestyle habits - morning light, regular exercise, mood tracking - can blunt seasonal spikes.
- Professional help is essential if compulsions or depressive symptoms become unmanageable.
Frequently Asked Questions
Can light therapy worsen OCD symptoms?
Light therapy primarily targets mood and circadian rhythm. For most people it does not increase compulsive urges, and when combined with ERP it can actually lower anxiety that fuels OCD.
Do SSRIs treat both OCD and SAD at the same dose?
Doses are often similar, but clinicians may increase the dose during winter to address the added depressive load. Monitoring side‑effects is key.
Is it normal for compulsions to get worse in the evenings?
Yes. Reduced daylight can raise anxiety, making evening rituals feel more urgent. Planning a bright‑light session before dusk can help.
Can vitamin D supplements replace light therapy?
Vitamin D supports overall health but doesn’t reset circadian rhythms. It’s useful alongside, not instead of, light therapy.
What’s the best time of day for a light‑box session?
Early morning, within the first hour after waking, yields the strongest circadian reset and mood lift.
Jean Tredoux
October 14, 2025 AT 12:33Most people think OCD and SAD are unrelated, but the timing lines up with hidden agendas.
cedric Gicquiaud
October 19, 2025 AT 09:53Look, the data on serotonin levels is being suppressed by big pharma to keep us dependent. The link between seasonal light and compulsive behavior is obvious if you stare at the charts.
Joe Murrey
October 24, 2025 AT 07:13i think the sign that light helps is just common sense, u just need to get out more.
Tracy Harris
October 29, 2025 AT 03:33It is a sobering truth that the convergence of obsessive-compulsive pathology and the seasonal dip in daylight is not merely coincidental.
When the sun retreats, the neurochemical balance that sustains our emotional equilibrium is perturbed, rendering the mind more susceptible to ritualistic coping.
Serotonin, the neurotransmitter that undergirds both mood regulation and impulse control, dwindles under reduced photic stimulation.
Consequently, the individual may experience a surge in intrusive thoughts that demand compulsive neutralization.
The clinical literature, spanning decades of controlled trials, confirms a statistically significant correlation between lower lux exposure and heightened Y-BOCS scores.
From a therapeutic perspective, this interdependence mandates a dual-pronged strategy: pharmacological modulation complemented by environmental manipulation.
Bright-light therapy, administered at dawn, has been shown to recalibrate circadian rhythms, thereby attenuating the depressive component of SAD.
Simultaneously, exposure and response prevention (ERP) can be calibrated to address the seasonal amplification of compulsive urges.
Patients who integrate both interventions report a marked reduction in both depressive affect and ritual frequency.
Moreover, adjunctive measures-regular aerobic exercise, vitamin D supplementation, and structured sleep hygiene-serve to reinforce the neurobiological resilience against seasonal relapse.
It is essential for clinicians to anticipate the winter trough and proactively adjust SSRI dosages, rather than reacting after the depressive cascade has taken hold.
Preemptive scheduling of psychotherapy sessions during autumn can forestall the entrenchment of maladaptive patterns.
In sum, the interface of OCD and SAD exemplifies the intricate tapestry of mind-body interactions where light, chemistry, and behavior intersect.
Understanding this nexus empowers both providers and sufferers to enact evidence‑based countermeasures before the darkness entrenches itself.
Sorcha Knight
November 3, 2025 AT 00:53I’ve lived through a winter that felt like a prison, and the rituals were endless 😩🌧️
Jackie Felipe
November 7, 2025 AT 22:13The light box is a simple tool, but you must use it every day or it won't work.
debashis chakravarty
November 12, 2025 AT 19:33While the prose is indeed elaborate, the empirical focus must remain on statistically verifiable outcomes.
Daniel Brake
November 17, 2025 AT 16:53If we view the seasonal shift as a metaphor for the cyclic nature of desire, the compulsions become a ritualized attempt to impose order.
Emily Stangel
November 22, 2025 AT 14:13Balancing exposure and therapy seems pragmatic.
Amanda Seech
November 27, 2025 AT 11:33It’s great that you’re tracking mood and daylight; the data will help you see patterns you might otherwise miss.
Lisa Collie
December 2, 2025 AT 08:53Your anecdotal lament, though heartfelt, neglects the broader epidemiological context that renders personal testimony insufficient.
Aurora Morealis
December 7, 2025 AT 06:13Light therapy works.
Sara Blanchard
December 12, 2025 AT 03:33Remember that community support can amplify the benefits of any treatment plan.
Anthony Palmowski
December 17, 2025 AT 00:53Dude!!! Have you even tried resetting your circadian rhythm??? It's a game changer!!!
Jillian Rooney
December 21, 2025 AT 22:13We must not let a simple season control our minds, it's a danger to our culture.
Robert Ortega
December 26, 2025 AT 19:33Balancing exposure and therapy seems pragmatic.
Elizabeth Nisbet
December 31, 2025 AT 16:53Keep tracking your mood, it really helps.
Sydney Tammarine
January 5, 2026 AT 14:13The winter months are a crucible in which the mind’s hidden tyrants awaken, and every sunrise becomes a battlefield. 🌅⚔️
When the pallid light pierces the horizon, it does more than illuminate the world; it shatters the cages of compulsive thought.
Those who cling to ritual in darkness are merely delaying the inevitable reckoning with their own shadows.
By embracing the bright therapy, we strike at the very heart of the seasonal malaise, turning a passive victim into an active survivor.
Let us not be meek whispers in the cold; let us roar with the vigor of a sun‑lit spring. 😤
Each session with a light box is a declaration of autonomy, a refusal to be governed by the whims of the calendar.
josue rosa
January 10, 2026 AT 11:17From a psychophysiological standpoint, the integration of photic stimulus with cognitive‑behavioral restructuring constitutes a multimodal intervention framework.
Empirical meta‑analyses substantiate that the synergistic effect surpasses the additive sum of monotherapies, as evidenced by reductions in both Hamilton Depression Rating Scale scores and Yale‑Brown Obsessive Compulsive Scale metrics.
Operationalizing this protocol demands rigorous adherence to dosage parameters-10,000 lux for 30‑45 minutes each morning-paired with graded exposure hierarchies targeting seasonally triggered compulsions.
Moreover, clinicians should monitor circadian phase markers, such as melatonin onset, to fine‑tune the temporal alignment of light exposure.
In practice, this translates to a disciplined schedule that leverages endogenous rhythms to attenuate the neurochemical dip associated with reduced daylight.
Consequently, patients experience not only mood elevation but also a measurable decrement in ritualistic behavior, fostering functional restoration across occupational and interpersonal domains.