 Nov, 17 2025
Nov, 17 2025
Imagine waking up every morning to a kitchen counter covered in 12 different pill bottles. Then again at noon. Then again at 6 p.m. And before bed, another round. This isn’t a scene from a movie-it’s the daily reality for millions of older adults in the U.S. who take five or more medications. The problem isn’t just the number of pills. It’s the frequency. Seven or more doses a day? That’s not just inconvenient-it’s a recipe for missed pills, hospital visits, and worsening health.
Why Fewer Doses Make a Real Difference
People don’t skip meds because they’re forgetful. They skip them because the system is broken. A 2014 JAMA Internal Medicine study found that nearly 30% of patients were taking medications seven or more times a day. But only 15% organized their pills into four or fewer daily time blocks. That mismatch is the problem. Your body doesn’t care if you take a pill at 8 a.m. or 9 a.m.-but your brain does. Too many reminders, too many routines, too much mental load. Simplifying your regimen isn’t about cutting corners. It’s about aligning your medicine with your life. Studies show that reducing daily doses from four to two can boost adherence by 25%. For older adults, that means fewer falls from rushing to take pills, fewer ER trips from missed doses, and more confidence managing their health.Four Proven Ways to Cut Down Daily Doses
There’s no one-size-fits-all fix. But four strategies have been tested, proven, and used successfully in clinics across the country.1. Fixed-Dose Combinations (FDCs)
This is when two or more drugs are combined into a single pill. Think of it like a multivitamin for your chronic conditions. For example, instead of taking separate pills for high blood pressure and cholesterol, you might get one pill that contains both. About one-third of all successful simplifications use this method. It works best for conditions like HIV, heart failure, and type 2 diabetes. In one trial, HIV patients switched from a six-pill-a-day regimen to a single pill-and missed doses dropped from 12% to 4% monthly. But FDCs aren’t magic. If your doses need to be adjusted separately, combining them won’t work. Your doctor or pharmacist has to check if the doses match up safely.2. Once-Daily Dosing
Not every pill can be taken once a day. But many can. Extended-release versions of medications like statins, blood pressure drugs, and even some antidepressants now exist. These are designed to release slowly over 24 hours, so you only need one dose. The catch? It’s not always possible. Some drugs break down too fast. Others need to be taken with food or on an empty stomach. A 2018 study showed that even when patients stuck to once-daily antiretroviral therapy, their clinical outcomes didn’t improve-just their adherence. That’s still a win, but it means you can’t assume fewer doses automatically means better health. You need to monitor.3. Medication Synchronization
This one’s simple but powerful. Instead of refilling your prescriptions on different days each month, you get them all on the same date. One pharmacy visit. One copay. One reminder. No more running out of blood pressure pills because your refill was due a week before your diabetes meds. Studies show this cuts pharmacy visits by 60% and reduces gaps in therapy. It’s especially helpful for people on fixed incomes or with limited transportation. But it only works if your pharmacist is on board. Not all pharmacies offer it. Ask. If they say no, ask for a referral to one that does.4. Multi-Dose Compliance Packaging
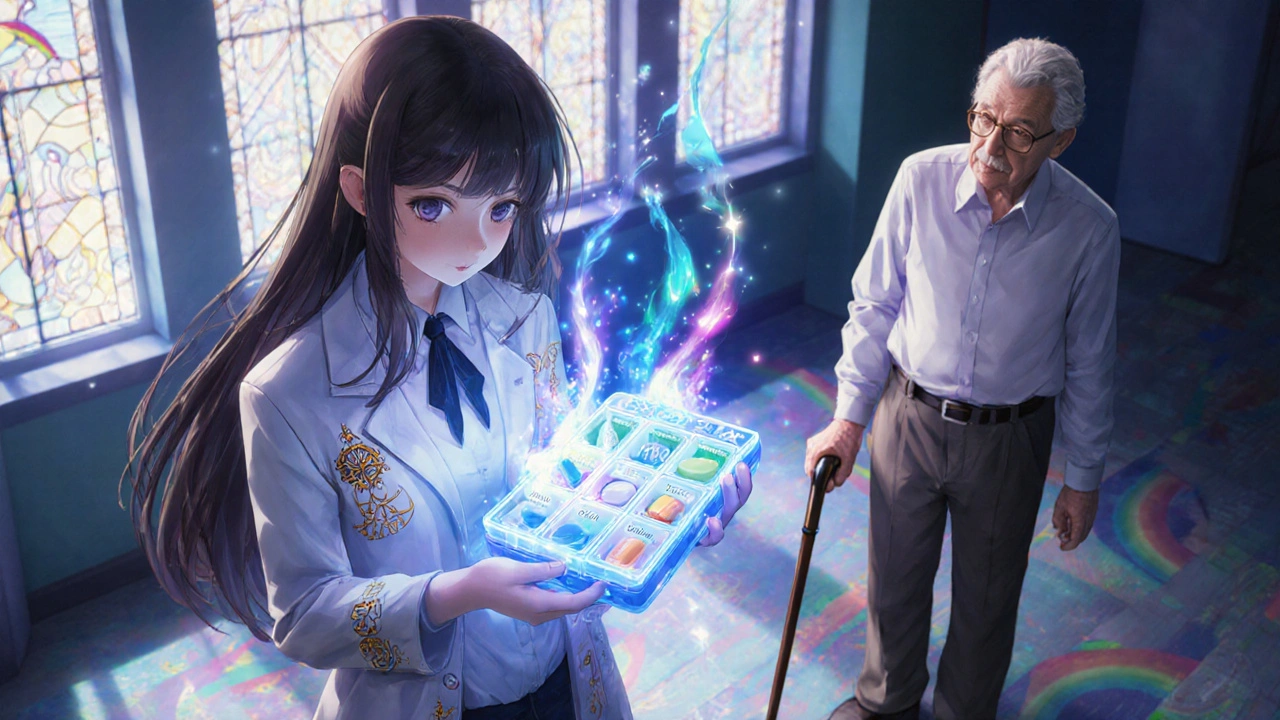
These are those little plastic boxes with compartments for morning, noon, evening, and bedtime. They’re not fancy, but they work. One study found patients using these had 22% better adherence than those using regular bottles. They’re a game-changer for people with memory issues, dementia, or caregivers managing multiple medications. One caregiver on AgingCare.com said, “My mother went from confusing her pills to knowing exactly what to take-without asking me every time.” But there’s a downside: cost. These boxes can add $15-$20 per month to your bill. And not all insurance covers them. Medicare Part D sometimes does-if you’re enrolled in a plan that includes medication therapy management.The Universal Medication Schedule (UMS)
You don’t need to invent a new routine. There’s already a standard: the Universal Medication Schedule. It breaks the day into four clear times:- Morning (7-9 a.m.)
- Afternoon (1-3 p.m.)
- Evening (6-8 p.m.)
- Bedtime (9-11 p.m.)
What Doesn’t Work-and Why
Not every drug can be simplified. Some diabetes meds need to be taken with meals. Some antibiotics must be spaced evenly. High-dose blood thinners can’t be combined with other pills without risking bleeding. A 2020 review of six studies found that simplification efforts for oral diabetes and hypertension meds often failed. Why? Because the drugs themselves don’t allow it. You can’t force a pill into a schedule that breaks its science. Also, don’t assume patients understand the new plan. One survey of 200 pharmacists found that 68% said patients misunderstood their simplified regimens. Some mixed up pills they thought were the same. Others took two pills together that shouldn’t be. Education is part of the process.How to Start-A Step-by-Step Plan
You don’t need a doctor’s appointment to begin. But you do need to be organized.- Make a full list. Write down every medication-prescription, over-the-counter, vitamins, supplements. Include the dose and how many times a day you take it.
- Bring it to your pharmacist. Pharmacists are medication experts. They see your full history. Ask: “Can any of these be combined? Can any be switched to once-daily versions?”
- Ask about insurance. If a new pill or packaging is recommended, ask: “Will my plan cover it?” If they say no, ask for an appeal form. Many insurers will approve it if you show it improves adherence.
- Try one change at a time. Don’t overhaul everything in a week. Start with the most burdensome part-maybe the 5 a.m. pill you always forget. Swap that first.
- Track for 30 days. Use a simple checklist or phone app. Note if you missed any doses. If adherence improves, keep it. If not, go back to the drawing board.

Who Should Lead This?
Too often, patients are left to figure this out alone. But it’s not their job. The best results come when doctors, pharmacists, and caregivers work together. A study found that when all three were involved, 50% of simplification recommendations were actually carried out. When only the pharmacist made the suggestion? Just 12%. If you’re a caregiver, take the lead. Print out the list. Go with the patient to appointments. Ask the questions. If you’re a patient, don’t be shy. Say: “This is too hard. Can we make it easier?”What’s Changing in 2025?
The tools are getting smarter. In 2022, the FDA approved 12 new fixed-dose combinations-up 25% from 2020. More are coming. Pharmacies are starting to use AI tools that scan your meds and suggest possible simplifications. Some Medicare Advantage plans are testing smart pill boxes that send alerts to your phone and your care team if you miss a dose. Medicare’s Annual Wellness Visit now includes a mandatory medication review. That means every year, you’re supposed to get a full check-up of your pills. Use it. Bring your list. Ask for simplification.It’s Not Just About Pills-It’s About Peace of Mind
Simplifying your regimen isn’t just a clinical goal. It’s a quality-of-life goal. Fewer pills mean less stress. Less confusion. More sleep. More time for the things you love. One woman in Wisconsin told her pharmacist, “I used to dread mornings. Now I take my one pill with coffee and feel like I’ve already won the day.” You don’t have to live with a cluttered counter and a heavy heart. The tools exist. The science backs it. The people who can help are right there-in your pharmacy, your clinic, your home. Start small. Ask one question. Try one change. Your future self will thank you.Can I just combine my pills myself if they look similar?
No. Never mix pills unless a pharmacist or doctor has approved it. Even if two pills look the same, they may have different active ingredients, release mechanisms, or interactions. Combining them without guidance can lead to overdose, underdose, or dangerous side effects. Always consult a professional before making any changes.
Does simplifying my meds mean I’ll get worse results?
Not if it’s done right. Studies show that when dosing frequency is reduced without changing the total daily dose, clinical outcomes stay the same-or improve-because you’re taking your meds more consistently. The real risk isn’t simplification; it’s skipping doses because the schedule is too complicated.
Will my insurance cover a once-daily version or a pill organizer?
It depends. Many Medicare Part D plans cover extended-release formulations if they’re medically necessary. Pill organizers are rarely covered, but some Medicare Advantage plans include them as part of medication therapy management programs. Always ask your pharmacist to check your plan’s formulary before switching.
How do I know if my regimen can be simplified?
If you’re taking four or more medications daily, or if you’re taking any drug more than twice a day, there’s likely room for simplification. Ask your pharmacist to run your list through a medication regimen complexity tool. Many pharmacies use digital tools that flag opportunities for fixed-dose combinations or once-daily switches.
What if my doctor says no to simplifying my meds?
Ask why. Sometimes it’s because the drug can’t be changed. Other times, it’s because they’re unaware of newer formulations. Request a second opinion from a pharmacist or geriatric specialist. You have the right to ask for safer, simpler options. If your current provider won’t help, find one who will.
Conor McNamara
November 19, 2025 AT 00:54i swear the gov't put this in the system so we forget our meds and go to the er more often... they make money off it. i took my bp pill at 8am and then again at 10am by accident last week and my head felt like a balloon. they dont care if you live or die as long as the bills keep coming in.
they dont want you healthy. they want you dependent.
Leilani O'Neill
November 20, 2025 AT 20:56How quaint. Americans have the luxury of having so many medications they need to organize them into a daily schedule. In Ireland, we don’t have the luxury of pharmaceutical overkill-we just get told to eat less sugar and walk more. This is not a ‘systemic problem’-it’s a cultural one. You’ve medicated your way out of personal responsibility.
Riohlo (Or Rio) Marie
November 22, 2025 AT 08:46Oh sweet mercy. Another ‘simplify your meds’ manifesto dripping with the saccharine optimism of someone who’s never had to juggle six prescriptions while caring for a dementia-stricken parent and working two jobs.
Let me guess-you’ve never had a pharmacist say ‘this combination could kill you’? No? Then you don’t get to speak on this. This isn’t a productivity hack. It’s a high-wire act performed with a blindfold and a loaded syringe. And now you want to ‘combine them’ like it’s a smoothie? Please.
The real tragedy isn’t the pill count-it’s that we’ve turned human biology into a spreadsheet.
steffi walsh
November 24, 2025 AT 01:30This made me cry. My grandma used to have 14 pills a day. Now she takes 3. She says she feels like she’s finally breathing again. Thank you for writing this. If you’re reading this and you’re overwhelmed-you’re not alone. Start small. One pill. One day. You’ve got this. 💪
Emanuel Jalba
November 25, 2025 AT 06:08THEY'RE LYING TO YOU. I saw a video on TikTok where a guy said the pharma companies invented all these extra pills just to keep you hooked. They don't want you healthy-they want you PAYING. I took my meds for 3 days and stopped. I feel better. I'm not a lab rat. 🚫💊
Heidi R
November 26, 2025 AT 09:47Of course you can't combine pills. That's why you need a professional. But why is it your pharmacist’s job to fix the mess your doctor made? You're not a puzzle to be solved. You're a person. And if your care team can't coordinate, that's negligence. Not convenience.
Brenda Kuter
November 26, 2025 AT 16:42My neighbor took a pill she thought was for blood pressure but it was actually for anxiety. She ended up in the ER. The pharmacist said she’d been taking them together for 6 months. No one checked. No one asked. I swear, if I didn’t do it all, my mom would be dead by now. They just hand out prescriptions like candy and then act shocked when people die.
It’s not about simplification. It’s about accountability.
Shaun Barratt
November 27, 2025 AT 06:57While the conceptual framework presented is broadly sound, empirical validation of dosage consolidation must be contextualized within pharmacokinetic parameters and individual metabolic variance. The assertion that adherence improvements equate to clinical benefit requires longitudinal cohort analysis, which is not uniformly represented in the cited literature. Furthermore, the assumption of homogeneity in patient comprehension neglects cognitive load theory and health literacy disparities. A standardized protocol, validated by peer-reviewed clinical trials, is warranted before widespread implementation.
Iska Ede
November 27, 2025 AT 13:51Oh wow. So the solution to 12 pills a day is... more pills? Just combine them into one big magic pill? Next you'll tell me we can just merge my insulin and my antidepressant into a chocolate bar. Maybe I'll just take a shot of whiskey instead. At least that's one dose and it makes me feel better. 🤡
Gabriella Jayne Bosticco
November 28, 2025 AT 05:41My mum used to have a drawer full of pills. We got her a pill organizer, and she started sleeping better. Not because the meds changed-but because she stopped feeling like a hospital. It’s not about reducing drugs. It’s about reducing chaos. You deserve to feel like yourself again, not a pharmacy.
Sarah Frey
November 28, 2025 AT 14:59The Universal Medication Schedule is an elegant solution grounded in behavioral psychology and clinical pragmatism. It reduces cognitive burden without compromising therapeutic integrity. However, its efficacy is contingent upon patient education, pharmacist involvement, and insurance coverage. Systemic adoption requires policy reform-not merely individual initiative. This is not a personal failure; it is a structural one.
Katelyn Sykes
November 28, 2025 AT 18:58My dad took 7 pills a day. We got him on a once-daily statin and a combo BP pill. Now he takes 2. He started walking again. He started cooking. He started laughing. It wasn’t magic. It was just… simpler. You don’t need a PhD to get this. You just need to ask the question: ‘Is this too hard?’ And then say ‘Let’s fix it.’
Pharmacist first. Doctor second. You last. You’re the most important part.
Gabe Solack
November 30, 2025 AT 14:33Just had my meds reviewed last week. My pharmacist caught that my diabetes med was overlapping with my heart med. We switched to a combo pill. Saved me $40/month and now I only take one thing at night. I didn’t even know I could ask. Don’t be shy. Pharmacists are the real superheroes here. 💊❤️