 Jan, 20 2026
Jan, 20 2026
Medication Risk Checker
Check Medication Risks for Elderly Patients
Enter a medication name to see if it's potentially risky for older adults based on the Beers Criteria guidelines.
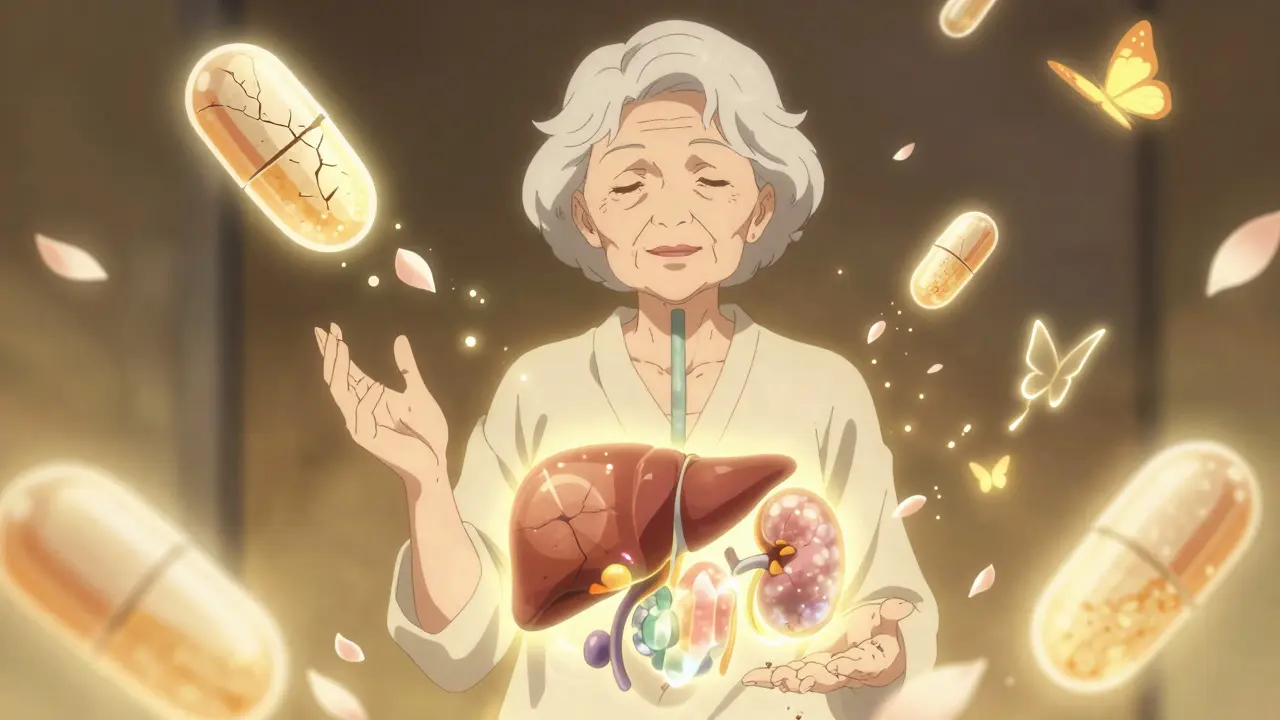
Older adults don’t just take more medications-they react to them differently. A pill that works fine for a 40-year-old can send a 75-year-old to the hospital. It’s not about taking too much. It’s about how the body changes with age, and how those changes turn ordinary drugs into hidden dangers.
Why Older Bodies Handle Drugs Differently
Your liver and kidneys don’t work the same after 65. Blood flow to the liver drops by 30-40% between ages 25 and 75. Kidneys filter less, too-glomerular filtration rate declines about 0.8 mL/min/1.73m² every year after 40. That means drugs stick around longer. What used to be a 12-hour effect can stretch into days.Body composition shifts, too. Fat increases while muscle decreases. That changes how drugs spread through the body. Lipid-soluble drugs like diazepam or chlordiazepoxide build up in fat tissue and release slowly, causing prolonged drowsiness, confusion, and falls. One study found that 20-30% of falls in seniors are directly tied to medication side effects.
It’s not just about dose. It’s about how the body processes the drug. A 70-year-old taking the same dose as a 30-year-old isn’t getting the same effect. They’re getting more-and for longer.
The Big Risk: Taking Too Many Pills
Polypharmacy-taking five or more medications at once-is common in older adults. Nearly half of people over 65 use five or more prescription drugs. Add over-the-counter painkillers, sleep aids, vitamins, and herbal supplements, and the number can jump to 10 or more.Each extra pill adds risk. Not just from the drug itself, but from how it interacts with others. Take NSAIDs like ibuprofen with blood thinners like warfarin? That combo triples the chance of a bleeding ulcer in seniors. Combine corticosteroids with NSAIDs? Risk of peptic ulcers goes up 15 times.
Even common combinations can be dangerous. Anticholinergic drugs-used for overactive bladder, allergies, or depression-can cause memory fog, dry mouth, constipation, and confusion. When stacked with other sedatives or antihypertensives, they can trigger delirium or falls. Many seniors don’t realize these symptoms aren’t normal aging. They think it’s just getting older. It’s not. It’s the meds.
High-Risk Medications to Watch Out For
The American Geriatrics Society’s Beers Criteria is the gold standard for identifying drugs that are risky for older adults. It’s updated regularly, and here are some key offenders:- Propoxyphene-a weak painkiller with strong side effects. It’s been pulled from the U.S. market, but some seniors still have old prescriptions.
- Indomethacin-an NSAID that causes more confusion and dizziness than others. Not worth the risk when safer options exist.
- Glyburide-a diabetes drug that can cause dangerous low blood sugar. Older adults don’t feel the warning signs as clearly, making hypoglycemia more likely to go unnoticed.
- Megestrol (Megace)-used for appetite stimulation, but linked to blood clots and fluid retention.
- Sliding-scale insulin-a reactive approach to diabetes that leads to erratic blood sugar swings. Fixed-dose regimens are safer.
- SSRIs like paroxetine-can increase fall risk by lowering sodium levels and causing dizziness.
Some drugs aren’t banned outright-they just need extreme caution. Acetylcholinesterase inhibitors (used for Alzheimer’s) can slow the heart too much in people with existing bradycardia. Glitazones for diabetes worsen heart failure. These aren’t “never use” drugs. They’re “use only if absolutely necessary, and monitor closely.”

Side Effects That Don’t Look Like Side Effects
Younger people notice nausea, rashes, or stomach pain. Seniors don’t. Their side effects are quieter-and more dangerous.- Falls-not just from dizziness. Sometimes from orthostatic hypotension caused by blood pressure meds.
- Memory lapses-could be anticholinergics, benzodiazepines, or even acid reflux meds like omeprazole.
- Weight loss-not always cancer. Could be loss of appetite from antidepressants or NSAIDs.
- Confusion or hallucinations-often mistaken for dementia. Pentazocine, diphenhydramine, and even some antibiotics can trigger this.
- Constipation-commonly blamed on diet. Could be from opioids, calcium channel blockers, or anticholinergics.
These aren’t normal aging. They’re red flags. If an older adult suddenly starts falling, forgetting names, or losing appetite, ask: What changed in their meds?
What Doctors and Pharmacies Should Be Doing
The Beers Criteria isn’t a rulebook. It’s a checklist. Every medication review should ask:- Is this drug still needed?
- Is there a safer alternative?
- Is the dose too high for age?
- Is this interacting with another drug?
- Is this causing symptoms we’re blaming on aging?
Pharmacists are critical here. Medication Therapy Management (MTM) programs-where pharmacists sit down with patients to review every pill-cut hospitalizations by up to 30%. But they’re underused. Only 1 in 5 seniors get a full med review each year.
Doctors need to stop prescribing in silos. A cardiologist adds a beta-blocker. A rheumatologist adds an NSAID. A neurologist adds an anticholinergic. No one sees the whole picture. A pharmacist or geriatrician needs to step in and connect the dots.

What Seniors and Families Can Do
You don’t need to be a doctor to protect yourself or a loved one.- Keep a real-time list-of every pill, supplement, and OTC drug. Include doses and why you’re taking them. Update it after every doctor visit.
- Bring the list to every appointment-even if it’s just for a cold. Don’t assume the doctor remembers what was prescribed six months ago.
- Ask: “Is this still necessary?”-If a drug was prescribed years ago for a now-cured condition, it might be time to stop.
- Report changes-If you feel more tired, dizzy, confused, or unsteady, say so. Don’t wait for your next checkup.
- Use one pharmacy-That way, the pharmacist can spot interactions across all your meds.
Many seniors don’t realize they can ask to deprescribe. It’s not giving up treatment. It’s removing what’s no longer helping-or what’s hurting more than helping.
The Bigger Picture: Why This Matters
By 2030, 1 in 5 Americans will be over 65. That’s 95 million people. Right now, 10-23% of hospital admissions in older adults are due to adverse drug reactions. Half of those are preventable.The cost? $3.5 billion a year in the U.S. alone. But money isn’t the real issue. It’s quality of life. It’s a fall that leads to a hip fracture. It’s confusion that leads to nursing home placement. It’s a loved one who used to garden and now can’t remember their own name.
Medications save lives. Vaccines, blood pressure pills, insulin-these are lifelines. But when we treat older adults like younger ones, we risk trading one problem for another. The goal isn’t to stop all meds. It’s to make sure every pill still earns its place.
Final Thought: It’s Not About Age. It’s About Biology.
A 70-year-old isn’t a 30-year-old with gray hair. Their body processes drugs differently. Their risks are different. Their symptoms are different.Respecting that difference isn’t ageism. It’s good medicine.
Why do elderly patients have more side effects from medications?
Older adults experience physiological changes that affect how drugs are absorbed, distributed, metabolized, and eliminated. Liver and kidney function decline, body fat increases, and muscle mass decreases. These changes cause drugs to stay in the body longer and build up to higher levels, increasing the risk of side effects like dizziness, confusion, and falls-even at standard doses.
What is the Beers Criteria and why is it important?
The Beers Criteria is a list of medications that are potentially inappropriate for older adults due to high risk of side effects or interactions. Published and updated by the American Geriatrics Society, it helps doctors avoid drugs that are more harmful than helpful in seniors. It’s used in hospitals, clinics, and nursing homes to guide safer prescribing and reduce preventable hospitalizations.
Can stopping a medication cause problems?
Yes, but only if done without medical supervision. Some drugs need to be tapered slowly to avoid withdrawal or rebound effects. The goal isn’t to stop all meds-it’s to stop the ones that are no longer needed or that cause more harm than benefit. Always work with a doctor or pharmacist before discontinuing any medication.
What are common signs that a medication is causing side effects in an elderly person?
Look for sudden changes: increased falls, confusion, memory loss, weight loss, constipation, dizziness, or new fatigue. These aren’t normal aging. They’re often signs that a medication is causing harm. Even mild symptoms like dry mouth or blurred vision can point to drug interactions or anticholinergic effects.
How can families help prevent dangerous drug reactions?
Keep a complete, up-to-date list of all medications-including supplements and OTC drugs-and bring it to every appointment. Ask the doctor: “Is this still necessary?” and “Could this be causing the symptoms we’re seeing?” Encourage the use of one pharmacy so all meds are tracked together. If a loved one is in a nursing home, ask about medication reviews and whether a pharmacist is involved in their care.
Kevin Narvaes
January 21, 2026 AT 23:41Sangeeta Isaac
January 22, 2026 AT 23:01Alex Carletti Gouvea
January 23, 2026 AT 04:15Philip Williams
January 24, 2026 AT 10:41Ben McKibbin
January 25, 2026 AT 10:05Melanie Pearson
January 25, 2026 AT 20:13Jerry Rodrigues
January 27, 2026 AT 07:49Uju Megafu
January 27, 2026 AT 10:43Jarrod Flesch
January 27, 2026 AT 23:07Kelly McRainey Moore
January 28, 2026 AT 17:11Stephen Rock
January 29, 2026 AT 05:37Amber Lane
January 30, 2026 AT 15:26Gerard Jordan
January 31, 2026 AT 16:23michelle Brownsea
February 1, 2026 AT 14:41