 Dec, 2 2025
Dec, 2 2025
When a patient walks out of the office with a new prescription, they’re not just getting a pill-they’re getting a promise. A promise that the medicine will work. That it won’t break their budget. That they can take it every day without fear or confusion. But too often, that promise gets broken-not because the drug doesn’t work, but because the patient doesn’t understand it.
Generic medications are one of the most powerful tools in modern healthcare. They’re safe, effective, and cost a fraction of brand-name drugs. In fact, 90% of all prescriptions filled in the U.S. are for generics, yet they make up only 23% of total drug spending. That’s billions saved every year. But here’s the problem: patients still hesitate. They worry. They stop taking their meds. And when they do, their health suffers.
Why Patients Doubt Generics
It’s not that people are irrational. It’s that they’ve been left with gaps in understanding.
Many patients notice their pill looks different. Maybe it’s a different color. Or shape. Or even has a weird marking on it. They remember the last time they took this drug-it was white and oval. Now it’s blue and round. They think: Is this the same thing?
Some have heard stories. My cousin took a generic and it didn’t work. Or worse: The pharmacy switched me without telling me. These aren’t just myths-they’re real concerns shaped by real experiences. And if a provider doesn’t address them, the patient assumes the worst.
A 2015 review in PMC found that despite decades of evidence showing generics are just as effective, many patients still believe they’re inferior. And that belief? It’s stronger than any clinical guideline.
What the Science Actually Says
The FDA doesn’t approve generics lightly. To get approval, a generic drug must prove it’s bioequivalent to the brand-name version. That means it delivers the same amount of active ingredient into the bloodstream at the same rate. The acceptable range? Between 80% and 125% of the brand’s performance. That’s not a guess. That’s science. Rigorous, repeatable, and tested on thousands of patients.
Yes, generics can have different inactive ingredients-fillers, dyes, coatings. But those don’t change how the drug works. They just change how it looks or tastes. And manufacturers must prove those differences don’t affect safety or effectiveness.
And the data backs this up. A 2019 report from the Association for Accessible Medicines analyzed 1.4 billion prescriptions. It found that patients were 266% more likely to abandon a brand-name drug than a generic one. Why? Cost. Ninety percent of generic copays were under $20. Only 39% of brand-name copays were that low.
When a patient can’t afford their medication, they skip doses. They split pills. They stop altogether. And then they end up back in the ER-costing far more than the drug ever would have.
Providers Are the Missing Link
Doctors and pharmacists aren’t just prescribers. They’re the most trusted source of health information patients have. A patient might not believe a drug ad. They might ignore a pamphlet. But when their provider says, This generic is just as good, they listen.
The American College of Physicians made it clear in 2022: doctors should prescribe generics whenever possible. Not because they’re cheap-but because they’re just as effective. And when cost is a barrier, prescribing a generic isn’t just smart-it’s ethical.
But here’s the catch: most providers don’t talk about it. A typical primary care visit lasts 13 to 16 minutes. There’s blood pressure to check, symptoms to review, follow-ups to schedule. Talking about pill color? It feels like a luxury.
Except it’s not.
When a patient stops taking their meds because they’re confused or scared, that’s not just a missed dose. It’s a failed treatment. It’s a hospital visit. It’s a higher cost down the line. Spending two minutes explaining why the pill looks different? That’s an investment. One that pays off in adherence, fewer complications, and better outcomes.

How to Talk About Generics-Without the Jargon
You don’t need to explain bioequivalence to a patient. You need to explain trust.
Here’s how to do it:
- Start early. Don’t wait for them to ask. When you prescribe a generic, say: “I’m prescribing this generic version because it’s just as effective as the brand, and it will save you a lot of money.”
- Address appearance. “You might notice this pill looks different from what you’ve taken before. That’s because it’s made by a different company. But the medicine inside is the same.”
- Normalize switching. “It’s common to switch between different generic brands over time. The FDA makes sure they all work the same way.”
- Connect cost to care. “If this costs you $15 instead of $80, you’re more likely to take it every day. And that’s what keeps you healthy.”
- Invite questions. “What worries you about this medication? I want to make sure you feel comfortable.”
Pharmacists play a huge role too. When a patient picks up a prescription and sees a different-looking pill, the pharmacist is often the first person they ask. Training pharmacists to proactively explain the switch-not just answer questions-is critical.
When Generics Aren’t the Answer
Not every drug can be swapped. Some medications have a narrow therapeutic index-meaning the difference between a helpful dose and a harmful one is tiny. For drugs like warfarin, levothyroxine, or certain anti-seizure medications, even small changes in absorption can matter.
The American Academy of Family Physicians is right to oppose mandatory substitution for these cases. But that doesn’t mean generics are bad. It means we need to be smarter.
The solution? Not blanket bans. Not silence. Personalized decision-making. If a patient has been stable on a brand-name drug for years, and switching causes problems, don’t force it. But if they’re struggling to afford it? Offer the generic-and monitor closely.
And if a patient is on a drug with a narrow therapeutic index? Make sure they’re on the same generic brand consistently. Don’t let them get switched back and forth between manufacturers without warning. That’s where confusion-and risk-creeps in.
The Bigger Picture: Cost, Access, and Equity
Generic drugs are a public health win. But recent trends are threatening that.
In 2023, the American Society of Health-System Pharmacists warned that prices for some essential generic drugs are rising sharply. Insulin. Antibiotics. Blood pressure meds. In some cases, a generic that once cost $5 now costs $50. Why? Market consolidation. Supply chain issues. Fewer manufacturers.
This flips the script. Now, the solution isn’t just about switching to generics-it’s about protecting them. Providers need to watch for these price spikes. If a generic suddenly becomes unaffordable, they need to speak up. Advocate for alternatives. Push for policy changes.
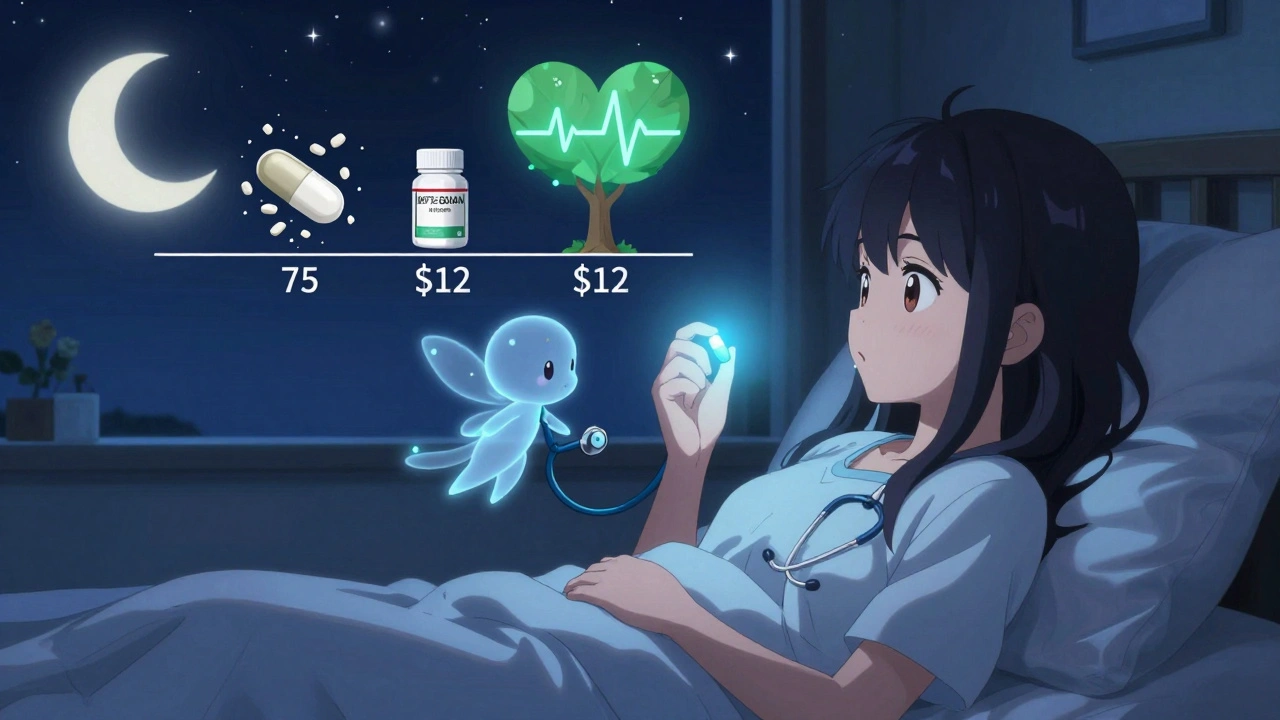
And when cost transparency tools in electronic health records flag a $75 brand vs. a $12 generic? Use that data. Don’t just click “prescribe.” Say something.
What Happens When Providers Stay Silent
Let’s say a patient with high blood pressure is prescribed a brand-name drug with a $75 copay. They skip doses. Their pressure stays high. Six months later, they have a stroke.
That’s not bad luck. That’s a system failure.
Providers who don’t talk about generics aren’t neutral. They’re complicit. Because silence sends a message: This drug is too expensive. Maybe you shouldn’t take it.
But when providers speak up? When they say, “This generic works just as well, and you can afford it,” they’re not just prescribing medicine. They’re restoring dignity. They’re giving patients control. They’re saving lives.
Final Thought: Advocacy Isn’t Optional
Generic drugs aren’t a compromise. They’re a cornerstone of affordable, effective care. And patient advocacy isn’t just about fighting for treatments-it’s about making sure patients can actually use them.
The science is clear. The data is solid. The cost savings are undeniable.
What’s left? The conversation.
It’s not about convincing patients to choose generics. It’s about helping them understand they’re already choosing the right one-when they’re given the facts.
So next time you write a prescription-take two minutes. Talk. Explain. Listen.
That’s not extra work. That’s the job.
Emmanuel Peter
December 2, 2025 AT 16:31Look, I get it, generics are cheaper, but I’ve seen people get sick because the generic didn’t work the same. My aunt took the generic levothyroxine and her TSH went through the roof. They told her it was ‘bioequivalent’-whatever that means-but she ended up in the ER. Science doesn’t always translate to real life.
Ashley Elliott
December 4, 2025 AT 08:40I’ve been a nurse for 18 years, and I’ve watched patients cry because they can’t afford their meds. I’ve had to explain, over and over, that the blue pill isn’t a different drug-it’s the same active ingredient, just made by a different company. It’s not about trust in the science-it’s about trust in the system. And if we don’t bridge that gap, we’re failing people.
Chad Handy
December 5, 2025 AT 13:37Let’s be real here-big pharma doesn’t want you to know this, but generics are often made in the same factories as the brand names, just without the marketing budget. The FDA’s bioequivalence standards are a joke. They allow 80% to 125% variation-that’s a 45% swing! If your blood pressure med varies that much, you’re basically playing Russian roulette with your heart. And don’t get me started on the fillers-some of those dyes and binders are linked to inflammation. You think your body doesn’t notice? It does. It just doesn’t scream until it’s too late.
Augusta Barlow
December 6, 2025 AT 09:59They say generics are safe, but who’s really checking? The FDA is understaffed, the labs are outsourced, and the manufacturers? They’re cutting corners to make more profit. I read a report once-back in 2017-that showed over 30% of generic manufacturers had FDA warning letters. And yet, we’re supposed to just trust that the blue pill is ‘just as good’? Please. My cousin’s kid had a seizure after switching to a generic seizure med. The hospital blamed ‘non-compliance.’ But the pharmacy switched it without telling anyone. That’s not a coincidence. That’s negligence.
Joe Lam
December 8, 2025 AT 09:44Wow. Just… wow. You wrote an entire essay on how to explain that a pill is the same. This isn’t a parenting manual. This is medicine. If your patient can’t grasp that a generic is bioequivalent, maybe they shouldn’t be managing their own meds. You’re infantilizing adults because you’re too lazy to teach them how to read a fact sheet. The real issue isn’t the pill-it’s the patient’s inability to engage with basic science.
Jenny Rogers
December 10, 2025 AT 03:30It is not merely a matter of cost-efficiency or pharmaceutical equivalence; it is a moral imperative to ensure that every individual, regardless of socioeconomic status, has equitable access to life-sustaining therapeutics. To withhold the truth-that generics are chemically identical-is to commit a form of epistemic violence against the vulnerable. One must not merely prescribe; one must sanctify the act of prescribing with ethical clarity and intellectual rigor.
Rachel Bonaparte
December 10, 2025 AT 14:59Okay, but what about the fact that most generics are made in China or India? And we all know what’s in the water there. I’ve seen videos-filthy factories, workers without gloves, raw chemicals just sitting in open bins. And the FDA inspects like… once every five years? So you’re telling me that the blue pill I just got is just as safe as the white one? That’s not science, that’s a gamble with my life. And don’t even get me started on the microplastics in the fillers. They’ve been found in 98% of generic pills. No one talks about that.
Scott van Haastrecht
December 11, 2025 AT 20:39This whole post is corporate propaganda dressed up as patient care. The real reason providers don’t talk about generics is because they’re pressured by pharmacy benefit managers to push them. It’s not about helping patients-it’s about hitting quotas. I work in a clinic where they get bonuses for prescribing generics. And guess what? We have patients showing up with broken pills because the cheap ones crumble. That’s not bioequivalence-that’s shoddy manufacturing. Stop pretending this is altruism. It’s profit.
Chase Brittingham
December 12, 2025 AT 16:11I’ve been on a bunch of generics over the years-blood pressure, cholesterol, even antidepressants-and honestly? I never noticed a difference. But I get why people freak out. When you’re sick, your body feels like a stranger. So when the pill looks different? It feels like betrayal. I think the key isn’t just explaining the science-it’s acknowledging the fear. Just saying, ‘I know this looks weird, and it’s okay to be unsure,’ goes a lot further than a lecture on bioavailability.
Bill Wolfe
December 13, 2025 AT 02:33Let’s be honest-this whole ‘generic is just as good’ narrative is a cult. The FDA is a puppet of Big Pharma. They approve generics with the same active ingredient, yes-but what about the excipients? The talc? The magnesium stearate? Those aren’t inert. They’re designed to slow absorption, to make the drug ‘last longer’-which means the peak concentration is lower. That’s not bioequivalence. That’s manipulation. And the fact that you’re telling people to just trust the system? That’s how people die. You’re not an advocate-you’re a cheerleader for a broken machine.
Benjamin Sedler
December 14, 2025 AT 18:15What if the real problem isn’t the pill? What if it’s that we’ve turned medicine into a commodity? We don’t care about the patient’s experience anymore-we care about the algorithm that says ‘generic preferred.’ I once had a doctor switch me from brand to generic and then say, ‘It’s the same, don’t worry.’ No, it’s not the same. The brand made me feel like someone cared. The generic made me feel like I was a line item in a spreadsheet.
zac grant
December 15, 2025 AT 17:00From a pharmacokinetic standpoint, the 80-125% bioequivalence window is actually quite robust when you consider inter-individual variability in metabolism. The CYP450 enzyme system varies by up to 30% between patients anyway, so the FDA’s range is conservative. The real issue is adherence, not bioequivalence. And the data is crystal clear: lower copays = better outcomes. Stop overcomplicating it. The science is settled.
michael booth
December 16, 2025 AT 09:31Carolyn Ford
December 17, 2025 AT 06:53You say providers are complicit for staying silent? What about the pharmacists? They’re the ones who switch the pill without telling you. I’ve had the same prescription for five years, and last month, I got a red capsule instead of white. No one said a word. I had to call the pharmacy myself. That’s not negligence-that’s malpractice. And now you want doctors to explain it? They didn’t even ask if I noticed.
Heidi Thomas
December 17, 2025 AT 22:11Generic manufacturers don’t even have to do full clinical trials. They just prove bioequivalence to the brand. That’s it. No long-term safety studies. No real-world data on 10-year outcomes. So how do you know it’s safe? You don’t. You just trust the system. And that’s exactly what they want you to do.
Rudy Van den Boogaert
December 19, 2025 AT 13:21I’ve been on a generic for my thyroid for years. Switched back and forth between brands. No issues. But I’ve also seen patients panic because the pill changed color. So I always say: ‘This is the same medicine, just a different look. Like a different brand of soda-same taste, different bottle.’ Works every time. No jargon. Just clarity. And yeah, it takes two minutes. But those two minutes? They’re worth it.