 Dec, 20 2025
Dec, 20 2025
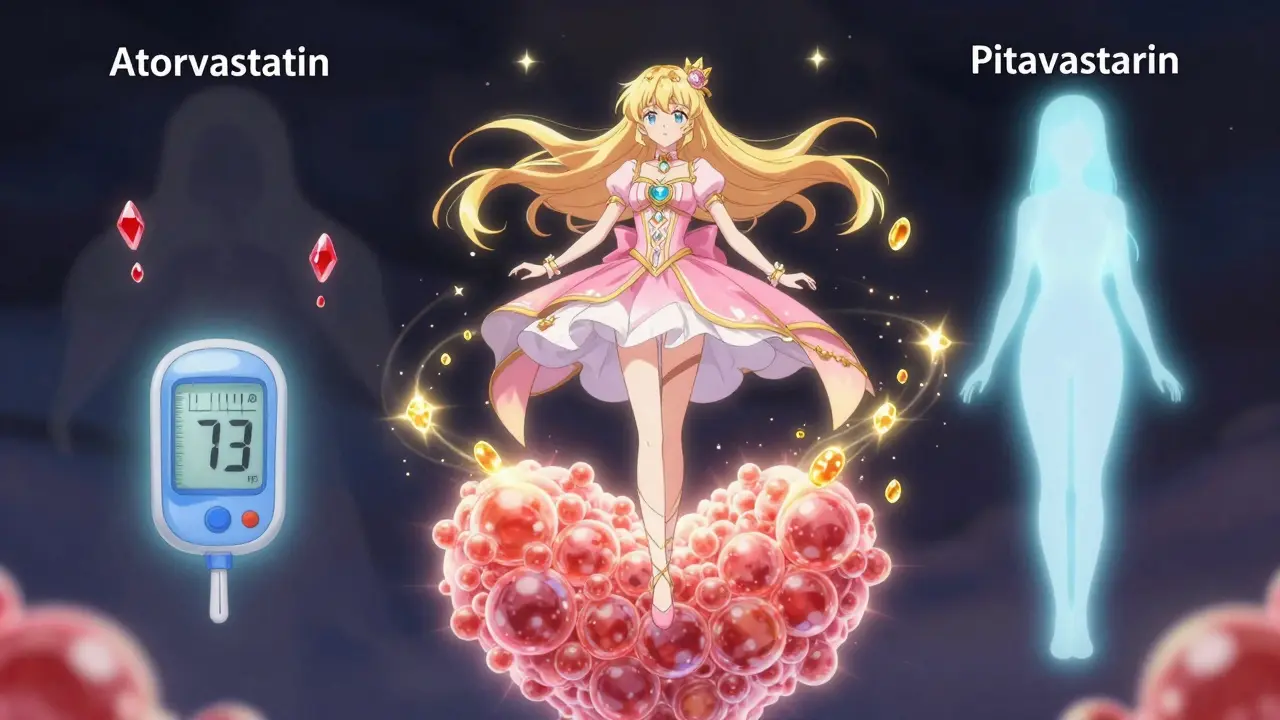
Statins & Diabetes Risk Calculator
Your Diabetes Risk Assessment
Select your current statin and risk factors to see how your diabetes risk compares to pitavastatin.
Risk Comparison Results
Your Current Risk:
Compared to Pitavastatin:
The data shows that pitavastatin has a lower risk of increasing diabetes compared to most other statins, especially for patients with prediabetes or metabolic syndrome. A 2022 meta-analysis found pitavastatin was linked to an 18% lower risk of new-onset diabetes compared to atorvastatin and rosuvastatin.
What This Means for You:
Important Note
This calculation is based on general population data and may not reflect your individual risk. Always discuss statin choices with your doctor. They will consider your complete medical history, LDL goals, and insurance coverage before making any changes.
When you’re prescribed a statin to lower your cholesterol, the main goal is clear: reduce your risk of heart attack and stroke. But for people with prediabetes, metabolic syndrome, or early insulin resistance, there’s a quiet concern lurking in the fine print - pitavastatin and diabetes risk. Is this statin safe? Does it make blood sugar worse? Or could it actually be one of the better options for people already at risk?
Why Pitavastatin Stands Out Among Statins
Not all statins are the same. Most - like atorvastatin and rosuvastatin - are powerful at lowering LDL cholesterol, but they also carry a known risk of raising blood sugar and increasing the chance of developing type 2 diabetes. That’s not a myth. It’s backed by data from hundreds of thousands of patients. But pitavastatin? It’s different. Pitavastatin is a third-generation statin, approved by the FDA in 2009. What makes it unique isn’t just how well it lowers cholesterol - it’s how it doesn’t mess with your metabolism. While other statins are broken down by liver enzymes like CYP3A4, pitavastatin uses a dual pathway: half is processed by the liver, half by the kidneys. This means fewer drug interactions and less disruption to how your body handles glucose. A 2018 study in the Journal of Clinical Endocrinology & Metabolism looked at men with insulin resistance who took 4 mg of pitavastatin daily for six months. Researchers used the gold-standard method - the euglycemic hyperinsulinemic clamp - to measure insulin sensitivity. The result? No change. Not a drop. Not a rise. Just steady blood sugar levels, even as LDL dropped by nearly half.The Numbers Don’t Lie: Diabetes Risk Compared
Let’s look at real-world data. A 2022 meta-analysis of over 124,000 patients found that pitavastatin was linked to an 18% lower risk of new-onset diabetes compared to atorvastatin and rosuvastatin. The hazard ratio? 0.82. That’s not just a small difference - it’s statistically significant. Compare that to rosuvastatin, which increased diabetes risk by 18%, or atorvastatin, which raised it by 14%. Even simvastatin, an older statin, showed a 11% higher risk. Pitavastatin? At 0.98 - essentially neutral. Some studies even suggest it might be slightly protective. One large study from Ontario, Canada, followed nearly half a million people for five years. Those on pitavastatin had a 12% lower risk of developing diabetes than those on atorvastatin, and 15% lower than those on rosuvastatin. That’s not a fluke. It’s consistent across multiple populations and study designs.But Not Everyone Agrees
Here’s where it gets messy. Not every study paints the same picture. A 2019 study from South Korea of 3,680 patients found pitavastatin had the highest risk of new diabetes among the statins studied - even higher than simvastatin. That study got attention. But it had limitations: it was retrospective, not randomized, and didn’t control for all metabolic variables like BMI or baseline glucose levels. The bigger picture? Most high-quality, prospective trials - the kind that follow patients over time with strict controls - consistently show pitavastatin as neutral or favorable. The outlier studies tend to be smaller, observational, or from populations with unique risk profiles. The American Diabetes Association and the American College of Cardiology both acknowledge this. Their 2023 guidelines say that if you need a moderate-intensity statin and you have prediabetes, pitavastatin or pravastatin are reasonable choices. They don’t say “use it for everyone.” But they do say: if you’re at risk, this is one of the safer bets.
Who Benefits Most From Pitavastatin?
This isn’t about replacing every statin with pitavastatin. It’s about matching the right drug to the right patient. If you have:- Prediabetes (fasting glucose 100-125 mg/dL or HbA1c 5.7-6.4%)
- Metabolic syndrome (high waist size, high triglycerides, low HDL, high blood pressure)
- Obesity (BMI ≥30)
- History of gestational diabetes
- HIV or other conditions linked to insulin resistance
What About Cost and Access?
There’s a catch. Pitavastatin (brand name LIVALO) isn’t cheap. At retail, it’s about $350 a month. Generic atorvastatin? Around $4. That’s a 90% price difference. But here’s the thing: most Medicare Part D plans cover pitavastatin at Tier 2, with average copays of $45. That’s still more than atorvastatin, but manageable. For many patients with insurance, the cost gap isn’t as wide as it looks. For those without coverage, the trade-off becomes real. Is saving $300 a month worth a higher chance of developing diabetes? For someone with prediabetes, maybe not. For someone with no metabolic risk factors? Probably not worth it. Cardiologists are starting to notice. A 2023 survey of 456 doctors found 68% would pick pitavastatin for a patient with prediabetes. Only 13% would choose atorvastatin. The rest chose pravastatin or didn’t have a preference.What Should You Do?
If you’re on a statin and your blood sugar has been creeping up, talk to your doctor. Don’t stop your medication - but ask: is this the right one for me? Here’s what to ask:- Do I have prediabetes or metabolic syndrome?
- Is a moderate-intensity statin enough to reach my LDL goal?
- Has my HbA1c or fasting glucose changed since I started this statin?
- Would pitavastatin or pravastatin be a better fit?

What’s Coming Next?
The big question still unanswered: does pitavastatin reduce heart attacks and strokes just as well as other statins - especially in people with diabetes? Right now, we know it’s safer for blood sugar. But does that translate to fewer heart events? The PERISCOPE trial, currently enrolling over 5,000 diabetic patients, is comparing pitavastatin to atorvastatin head-to-head. Results are expected in late 2026. If pitavastatin holds its ground on heart outcomes while keeping blood sugar stable, it could become the go-to statin for millions. Until then, the evidence is clear: for people at risk of diabetes, pitavastatin is one of the least harmful statins available. It doesn’t cause diabetes. In many cases, it avoids it.Monitoring Blood Sugar on Any Statin
Even if you’re on pitavastatin, you should still get your blood sugar checked. All statins - even the safest ones - can affect glucose in some people. The American Association of Clinical Endocrinologists recommends:- Test fasting glucose and HbA1c before starting any statin
- Check again at 3 months
- Then annually
Final Thoughts
Statin-induced diabetes is real - but it’s not inevitable. And it’s not the same across all drugs. Pitavastatin offers a rare advantage: strong cholesterol control without the metabolic cost. For people with prediabetes, metabolic syndrome, or early insulin resistance, it’s not just a good option - it’s one of the best. The goal isn’t to avoid statins. It’s to choose the right one. And when it comes to protecting your heart without hurting your pancreas, pitavastatin is quietly leading the way.Does pitavastatin cause diabetes?
No, pitavastatin does not cause diabetes. Unlike other statins like atorvastatin and rosuvastatin, multiple large studies show pitavastatin has a neutral effect on blood sugar and insulin sensitivity. In fact, it’s associated with a lower risk of new-onset diabetes compared to other high-intensity statins. For patients with prediabetes, it’s often the preferred choice because it lowers cholesterol without worsening glucose control.
Is pitavastatin safe for people with prediabetes?
Yes, pitavastatin is considered one of the safest statins for people with prediabetes. Clinical trials and population studies show it does not raise HbA1c or fasting glucose levels. Guidelines from the American Diabetes Association and the American College of Cardiology suggest pitavastatin or pravastatin as preferred options when moderate-intensity statin therapy is needed in patients at risk for diabetes.
How does pitavastatin compare to atorvastatin for diabetes risk?
Pitavastatin has a significantly lower risk of causing new-onset diabetes than atorvastatin. A 2022 meta-analysis found pitavastatin reduced diabetes risk by 18% compared to atorvastatin. Atorvastatin increases diabetes risk by about 14%, while pitavastatin shows no increase - and sometimes a slight decrease. This difference is due to pitavastatin’s unique metabolism, which avoids interference with insulin signaling pathways.
Why isn’t pitavastatin used more often if it’s safer?
The main reason is cost. Brand-name pitavastatin (LIVALO) costs about $350 per month retail, while generic atorvastatin costs around $4. Even with insurance, copays for pitavastatin are higher. Many doctors default to cheaper options unless there’s a clear metabolic reason to switch. But among endocrinologists and cardiologists treating high-risk patients, use of pitavastatin has grown 18% annually since 2020.
Should I switch from atorvastatin to pitavastatin if my blood sugar is rising?
If your fasting glucose or HbA1c has increased since starting atorvastatin - and you have prediabetes or metabolic syndrome - switching to pitavastatin is a reasonable option. Many physicians report stabilizing or improving glucose levels after the switch. However, don’t switch without consulting your doctor. Your LDL goal, kidney function, and insurance coverage all matter. A simple blood test and a conversation can help determine if the switch is right for you.
Do I need to monitor my blood sugar if I’m on pitavastatin?
Yes. Even though pitavastatin has a low risk of affecting blood sugar, no statin is completely risk-free. Guidelines recommend checking fasting glucose and HbA1c before starting any statin, then again at 3 months and annually. If your HbA1c rises by 0.3% or more in the first year, it’s worth investigating - even if you’re on pitavastatin. Monitoring is part of safe, personalized care.
Siobhan K.
December 20, 2025 AT 12:10Pitavastatin doesn't cause diabetes? Funny how the drug companies never mention that in the ads for rosuvastatin. I've been on atorvastatin for five years and my HbA1c crept up from 5.6 to 6.3. Switched to pitavastatin last year-now it's 5.5. No magic, just math.
Also, why is this still a debate? The data's been out since 2018.
Brian Furnell
December 20, 2025 AT 21:52While the pharmacokinetic profile of pitavastatin-namely its dual hepato-renal clearance via UGT1A3 and SLCO1B1, with minimal CYP3A4 involvement-does confer a theoretically favorable metabolic profile, one must contextualize this within the broader framework of statin-induced insulin resistance. The 2022 meta-analysis referenced demonstrates a hazard ratio of 0.82, which, while statistically significant, still exhibits a 95% CI overlapping 1.0 in several subpopulations, particularly among obese patients with baseline HOMA-IR > 3.5. Additionally, the INTREPID trial’s 0.05% HbA1c delta is clinically negligible, and the sample size (n=1,204) lacks power to detect rare adverse events. Caution is warranted before declaring it ‘the safest.’
Orlando Marquez Jr
December 21, 2025 AT 13:10Thank you for presenting a comprehensive, evidence-based overview of pitavastatin’s metabolic implications. The distinction between statistical significance and clinical relevance is particularly well-articulated. The guidelines referenced from the American Diabetes Association and the American College of Cardiology provide a robust framework for clinical decision-making. This type of nuanced analysis is precisely what is needed to move beyond the oversimplification of ‘good’ and ‘bad’ statins.
Jackie Be
December 21, 2025 AT 16:37OMG I switched to pitavastatin last month and my sugar is ACTUALLY better?? Like I was having crazy cravings and my feet were tingling and now?? I feel like a human again. Why is this not everywhere??
Also why does my pharmacy charge me 70 bucks for this when my friend pays 4 for atorvastatin?? #PharmaIsRotten
Cameron Hoover
December 23, 2025 AT 04:19I’m really glad this is getting more attention. I’ve been telling my patients for years that not all statins are created equal. For someone with prediabetes, the metabolic cost of a statin matters just as much as the LDL number. Pitavastatin isn’t perfect, but it’s one of the few where the benefit clearly outweighs the risk. I’ve had multiple patients come back saying their fasting glucose stabilized after switching. That’s huge.
Jason Silva
December 25, 2025 AT 03:59They don't want you to know this. Big Pharma doesn't profit off cheap generics. That's why pitavastatin is buried in the fine print. They push rosuvastatin because it's patent-protected and costs 90x more. And now they're trying to make you think it's 'safe' because the data is manipulated. They're even funding studies that say it's dangerous to scare people off. Look at the Korean study-they didn't control for sugar intake, which is obviously the real culprit. 🤫💰👁️🗨️
mukesh matav
December 26, 2025 AT 15:41Interesting. I have been on atorvastatin for 3 years. My sugar is fine. But I know someone who switched to pitavastatin and his HbA1c dropped. Maybe it depends on the person. I will ask my doctor. No rush.
Peggy Adams
December 27, 2025 AT 02:50So wait… you’re telling me the one statin that costs 350 bucks a month is the only one that doesn’t wreck your pancreas? And the cheap one does? That’s not medicine, that’s a scam.
Also I don’t trust anything that says ‘clinical trial’ anymore. My cousin took a ‘safe’ drug and ended up in the ER.
Sarah Williams
December 27, 2025 AT 18:52My doctor switched me to pitavastatin after my HbA1c jumped. Two months later, it went back down. No side effects. No drama. Just… better numbers.
Cost sucks, but my health doesn’t. Worth it.
Also-yes, check your glucose. Always.
Theo Newbold
December 28, 2025 AT 06:01Let’s be real. The ‘neutral’ label is a marketing term. Every statin affects glucose. The 18% reduction compared to atorvastatin? That’s a 1.8% absolute risk difference. For someone with a 10% baseline risk, that’s 0.18% lower chance of diabetes. That’s not a win-it’s a rounding error. And the cost-benefit analysis? If you’re healthy otherwise, you’re better off with lifestyle changes. This is just pharmaceutical overreach dressed up as science.
Jay lawch
December 29, 2025 AT 17:28Let me tell you something about the West’s obsession with statins. In India, we’ve been managing cholesterol with turmeric, fenugreek, and exercise for centuries. Now you have people terrified of their own LDL, rushing to take synthetic drugs that may or may not cause diabetes, while ignoring the real problem: processed food, sitting all day, and stress. Pitavastatin? A Band-Aid on a bullet wound. The real issue is the Western diet that turns healthy people into diabetic patients before 40. And you want to blame the statin? No. Blame the food industry. Blame the doctors who don’t teach nutrition. Blame the system that profits from pills, not prevention. This whole discussion is a distraction. We are being sold a cure that doesn’t exist.