 Dec, 27 2025
Dec, 27 2025
When a child swallows a handful of pills by accident, or an adult takes the wrong dose of a prescription by mistake, seconds matter. The poison control hotline is there-24/7, free, and ready to help. You don’t need to wait for symptoms. You don’t need to drive to the ER. You just call 1-800-222-1222. And in most cases, you’ll get expert advice that keeps you out of the hospital.
How the Poison Control Hotline Actually Works
The poison control hotline isn’t just a phone number. It’s a nationwide network of 53 accredited centers, all connected through the National Poison Data System (NPDS), the only real-time poisoning surveillance system in the U.S. When you dial 1-800-222-1222, your call is automatically routed to the center closest to you based on your area code. You’re connected to a Specialist in Poison Information (SPI)-usually a pharmacist, nurse, or doctor with years of toxicology training. These specialists don’t guess. They use 1,540 evidence-based algorithms developed over decades of research. Each one is built around a specific substance-like acetaminophen, ibuprofen, or antidepressants-and accounts for factors like age, weight, amount taken, and time since ingestion. For medication exposures, which make up nearly half of all calls, the system checks for drug interactions, liver toxicity risks, and therapeutic index thresholds. The whole process takes 8 to 12 minutes on average. You can also text “poison” to 797979 or use the webPOISONCONTROL tool at poisonhelp.org. The online tool walks you through six key questions: what was taken, how much, when, your age, your weight, and your zip code. It gives you a risk assessment in under 3 minutes and has been shown to match human specialist advice 97.3% of the time.What to Report When It’s a Medication Emergency
Don’t say “I took some Tylenol.” That’s not enough. You need specifics.- Exact name: “Tylenol Extra Strength 500mg” not just “Tylenol.” Brand and generic names matter-some pills look alike but have different doses.
- Amount ingested: “Three 500mg tablets” or “15 pills from the bottle.” Estimate if you’re unsure, but be as close as possible.
- Time of ingestion: “About 2:15 PM” or “45 minutes ago.” Timing determines how the body is processing the drug.
- Patient details: Age, weight in kilograms (if you don’t know it, give pounds-specialists can convert), and any existing conditions like liver disease or pregnancy.
- Symptoms: “Nausea,” “drowsy,” “vomiting twice,” “rash on arms.” Even small changes matter.
- Other medications: “I’m also taking blood pressure medicine and Xanax.” Polypharmacy is a major risk-32% of serious cases involve drug interactions.

What Happens After You Call
Most calls-about 60%-are resolved at home. No ambulance. No ER. Just clear instructions: “Watch for vomiting,” “Give activated charcoal,” “Don’t induce vomiting,” or “Start N-acetylcysteine now.” For acetaminophen overdoses, they’ll schedule follow-up calls at 4, 8, and 24 hours to check liver enzyme levels. Ninety-two percent of those callbacks are completed successfully. If a hospital visit is needed, the specialist will tell you exactly where to go and what to bring. They’ll even call ahead to alert the ER so they’re ready. That’s because poison centers have formal agreements with nearly every U.S. hospital. Level I trauma centers are required to have a direct line to their local poison center. You’ll also get an email summary with everything discussed: the substance, dose, risk level, and instructions. About 78% of people keep that email as a reference. Some save it for their doctor’s visit. Others print it out for family members.Why This Service Saves Lives and Money
This isn’t just convenient-it’s life-saving and cost-effective. A 2019 study found poison control centers saved the U.S. healthcare system $1.8 billion a year by preventing unnecessary ER visits. For every dollar spent on poison control, society gains $7.67 in saved medical costs and lost productivity. The most common calls? Pediatric medication ingestions. Kids get into medicine bottles. Parents panic. But poison control prevents ER visits in 83% of these cases. One Reddit user-a pharmacist-shared how following hotline advice to give N-acetylcysteine within 8 hours saved a toddler from liver failure. That’s the kind of outcome that happens every day. And it’s not just kids. Opioid, sedative, and cardiovascular medication exposures have risen sharply since 2018. The system adapts: in 2022, protocols were updated for 27 new compounds, including synthetic opioids and weight-loss drugs with hidden toxicities.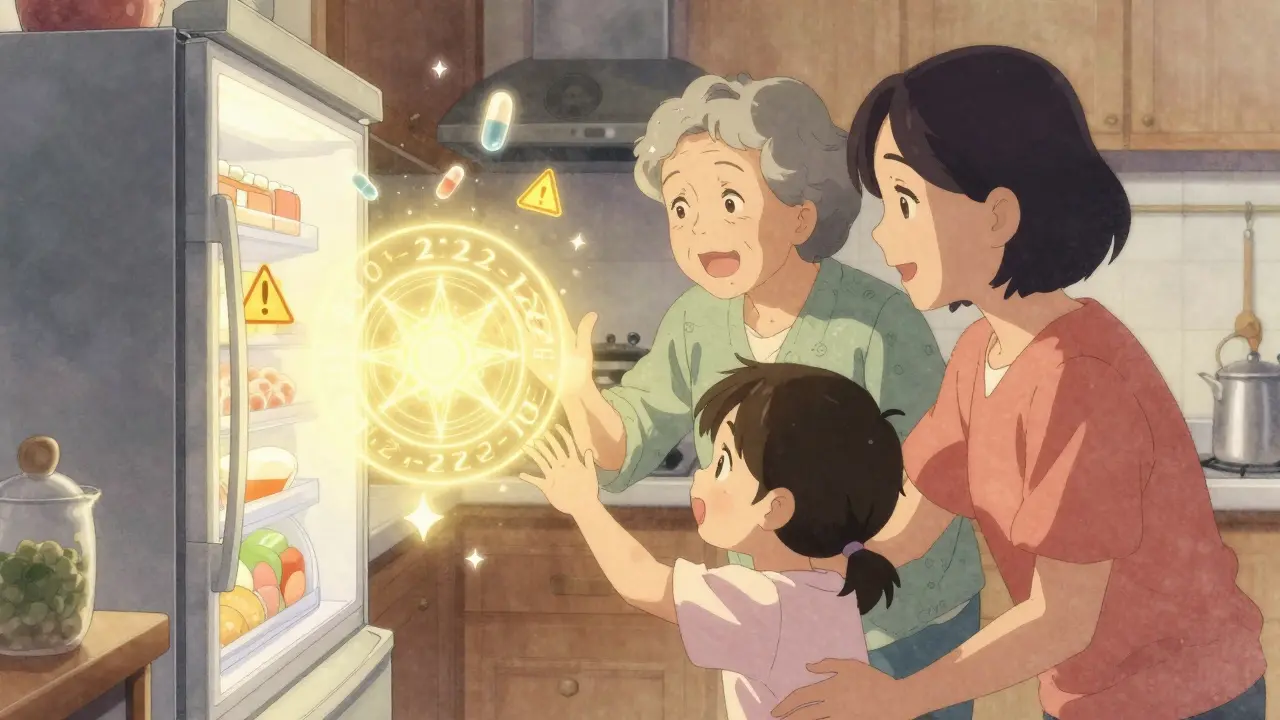
Limitations and What You Shouldn’t Rely On
The system is powerful, but not perfect. It doesn’t handle intentional overdoses or cases involving more than two substances. Those require a live call-never use the web tool alone if someone is unconscious, having seizures, or deliberately overdosing. Also, don’t wait for symptoms. If you think someone took something they shouldn’t have, call immediately. Many drugs, like acetaminophen or iron pills, don’t cause symptoms until damage is already done. Waiting can be fatal. And while the hotline is free and confidential, some hospitals have tightened privacy rules since 2018, which can delay follow-up information. But that doesn’t change your right to call. Your information is protected under HIPAA. No one will report you to authorities unless there’s evidence of child abuse or intentional harm.How to Be Ready Before It Happens
Don’t wait for an emergency to learn this. Keep the number 1-800-222-1222 saved in your phone. Post it on the fridge. Tell babysitters and grandparents. Make sure everyone who cares for kids knows it. Keep medicine locked up. Use child-resistant caps-even if they’re hard to open. And never transfer pills to unmarked containers. A pill that looks like a candy might be a dangerous dose. If you take multiple medications, keep a current list with names, doses, and why you take them. Bring that list to the ER if needed. Poison specialists will ask for it. And if you ever feel unsure-call. Even if it turns out to be nothing. Better safe than sorry. That’s why this service exists.Is the poison control hotline really free?
Yes. There is no charge to call 1-800-222-1222 or use webPOISONCONTROL. The service is funded by government grants, hospital support, and state funding. You don’t need insurance, identification, or a credit card. It’s available to anyone in the U.S. at any time.
Can I call poison control for my pet?
No. The poison control hotline is for human exposures only. For pets, contact the ASPCA Animal Poison Control Center at (888) 426-4435. There is a fee for that service, but it’s staffed by veterinary toxicologists who specialize in animal cases.
What if I don’t know what was taken?
Call anyway. Bring the container or bottle with you if you can. If it’s a pill, describe the color, shape, and any markings (like “M 30” or “20” on the tablet). Specialists can often identify unknown substances from photos or descriptions. Don’t wait to find out what it is-time matters.
Do I need to go to the ER after calling poison control?
Not always. In fact, most cases are managed safely at home. But if the specialist says to go, go immediately. They know when a substance is dangerous enough to need monitoring, IV treatment, or antidotes like N-acetylcysteine or flumazenil. Don’t second-guess their advice.
Is the poison control hotline available in Spanish or other languages?
Yes. The hotline offers translation services in over 150 languages. When you call, say the language you need, and an interpreter will join the call within seconds. The webPOISONCONTROL tool also supports multiple languages, including Spanish, Chinese, Vietnamese, and Arabic.
Can I call poison control for a suspected overdose that happened hours ago?
Yes. Even if it’s been several hours, call. Some medications, like extended-release opioids or antidepressants, cause delayed toxicity. Symptoms may not show up until 12-24 hours later. Poison specialists know how different drugs behave over time and can tell you whether to monitor at home or seek care.
What if I’m worried about being reported for an accidental overdose?
You won’t be reported. Poison control centers are confidential and non-judgmental. Their job is to save lives, not to punish. They won’t call the police, notify your employer, or share your information unless there’s clear evidence of child abuse, elder abuse, or intentional harm. Calling is the safest thing you can do.
Janice Holmes
December 28, 2025 AT 15:37OMG I JUST CALLED THEM WHEN MY KID ATE THREE OF MY XANAX-AND THEY DIDN’T JUDGE ME. THEY GAVE ME A STEP-BY-STEP PLAN WITH TIMING FOR ACTIVATED CHARCOAL AND A LIVER ENZYME CHECKLIST. I WAS CRYING, THEY WERE CALM. THIS SERVICE IS A GODSEND. 🙏
Alex Lopez
December 28, 2025 AT 16:43While the service is undeniably valuable, one must acknowledge that the 97.3% accuracy rate of webPOISONCONTROL is derived from a curated dataset with high-quality metadata inputs. Real-world user error-such as misidentifying pill markings or misreporting time of ingestion-can significantly degrade predictive fidelity. The algorithmic models, though robust, remain contingent on Garbage In, Garbage Out principles.
Robyn Hays
December 29, 2025 AT 23:28My grandma doesn’t use smartphones, so I printed out the poison control number and taped it to her fridge next to the microwave instructions. She calls them every time she’s confused about a new pill-once for a confused label on her blood pressure med. They talked her through it like she was family. That’s the kind of care we need more of. 💛
Babe Addict
December 31, 2025 AT 00:41Let’s be real-this whole system is just a glorified triage bot with a human voice. The '1,540 algorithms'? They’re just decision trees built from old case studies. And don’t get me started on 'N-acetylcysteine'-it’s not magic, it’s just a glutathione precursor. You still need to monitor labs. Stop acting like this is cutting-edge medicine.
Kylie Robson
January 1, 2026 AT 00:23Correction: The NPDS doesn't just track medication exposures-it integrates with CDC’s National Syndromic Surveillance Program and FDA’s MedWatch. The real-time data feeds into FDA risk assessments for new pharmaceuticals. If you think poison control is just 'answering phones,' you haven't read the 2023 White Paper on Toxicogenomic Surveillance. The infrastructure is more sophisticated than most hospital ERs.
Caitlin Foster
January 1, 2026 AT 00:31YOU CALL IMMEDIATELY!!! NO WAITING!!! I SAW A GUY WAIT 6 HOURS BECAUSE HE THOUGHT IT WAS 'JUST A BAD STOMACH'-AND HIS KID HAD IRON TOXICITY!!! THEY’RE NOT JUST A HOTLINE-THEY’RE A LIFELINE!!! SAVE THE NUMBER!!! TELL EVERYONE!!!
Andrew Gurung
January 2, 2026 AT 15:19Of course it's free-because it’s subsidized by Big Pharma’s lobbying dollars. They don’t want you going to the ER and getting expensive antidotes-they want you to stay home and take the 'recommended' NAC while they quietly adjust dosing guidelines. The real agenda? Preventing liability lawsuits. 😏
Elizabeth Ganak
January 3, 2026 AT 22:55in india we don’t have this but i wish we did. my cousin took wrong medicine and we drove 3 hours to hospital. no one told us what to do. i cried so hard. thank you for sharing this. maybe one day we can have something like this too.
Nicola George
January 5, 2026 AT 11:24Interesting how they say 'don't wait for symptoms'-but half the people who call are just paranoid moms who think their toddler licked a pill off the floor. I’ve heard the calls. 90% are non-emergencies. The system works, but it’s also a babysitter for the anxious middle class.
Raushan Richardson
January 6, 2026 AT 09:08I’m a nurse and I tell every new parent I meet: save this number. I had a mom text me last week because her baby swallowed a vitamin gummy-she called poison control first, got the all-clear, and didn’t panic. That’s the power of knowledge. Don’t wait until it’s too late. Keep it saved. Tell your sister. Tell your neighbor. It’s that simple.
Miriam Piro
January 8, 2026 AT 01:33Think about this: poison control centers are the only national system that doesn’t require insurance, ID, or a social security number. That’s not just healthcare-that’s a radical act of equity. But who really controls the data? The NPDS feeds into private health analytics firms. Your ingestion history is being sold to pharmaceutical companies to predict 'medication adherence patterns.' They know when you skipped your antidepressant. They know when you took too much. And they’re building behavioral profiles from your panic. This isn’t safety-it’s surveillance with a soothing voice.
dean du plessis
January 9, 2026 AT 03:32