 Jan, 30 2026
Jan, 30 2026
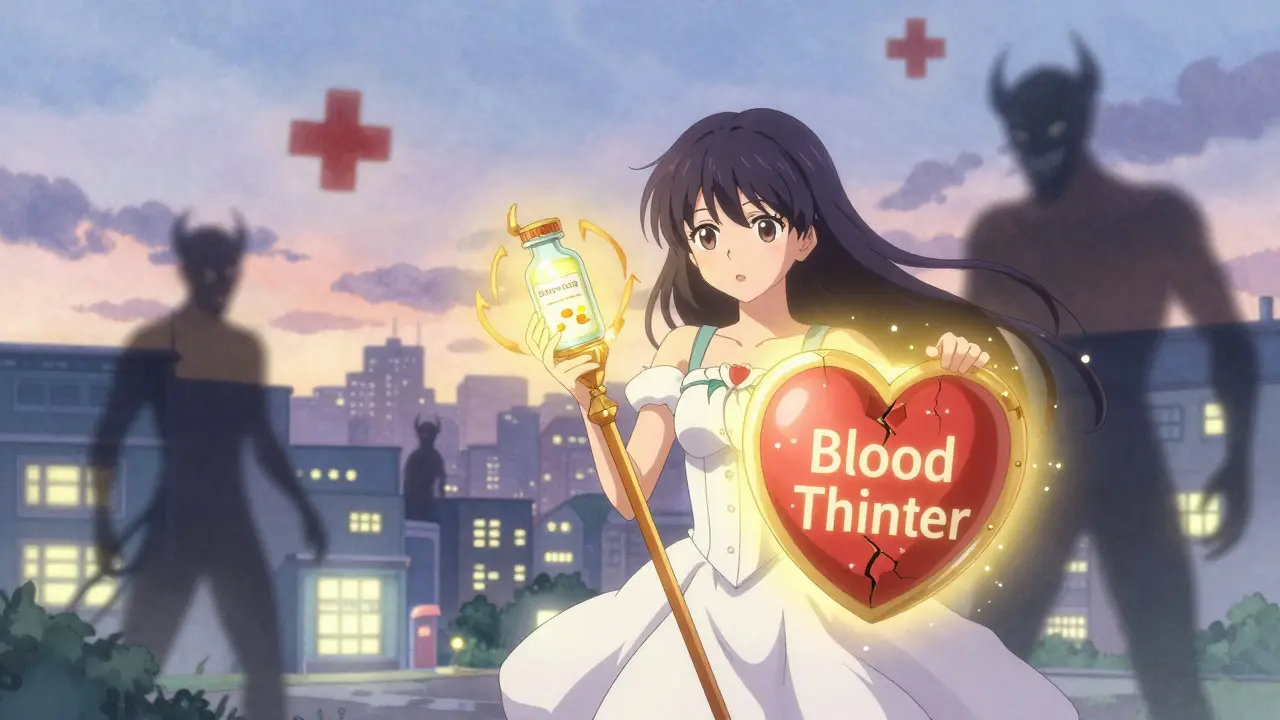
When you're on a blood thinner, even a simple headache remedy could put you in the hospital. Mixing common painkillers like ibuprofen or naproxen with anticoagulants isn't just a minor caution-it's a dangerous combo that can trigger severe, sometimes fatal, bleeding. This isn't theoretical. Real people, real hospitals, real deaths are tied to this interaction. And the data doesn't lie.
How Dangerous Is This Mix?
A massive 2024 study from Denmark tracked over 51,000 people on blood thinners for blood clots. The results were shocking. Those who also took NSAIDs were more than twice as likely to be hospitalized for bleeding. Not just stomach bleeds. Not just minor bruising. Bleeding-in the brain, lungs, kidneys, and gut. The risk wasn't the same across all NSAIDs. Naproxen raised bleeding risk by more than four times. Diclofenac? Three times higher. Even ibuprofen, often thought of as "milder," still doubled the chance of serious bleeding. These aren't small numbers. These are life-or-death odds. And it doesn't matter if you're on warfarin or one of the newer drugs like apixaban or rivaroxaban. The danger is the same. A lot of people assume the newer blood thinners are safer overall, but when paired with NSAIDs, they offer no protection. The combination breaks the body's ability to stop bleeding-no matter what anticoagulant you're using.Why Do These Drugs Clash?
Blood thinners work by slowing down your body's clotting system. Warfarin blocks vitamin K, while DOACs like apixaban directly inhibit clotting factors. That's their job-to prevent dangerous clots in the heart or legs. NSAIDs do something different but just as dangerous. They block enzymes called COX-1 and COX-2. COX-2 helps with inflammation and pain-that's why they work for arthritis or back pain. But COX-1 is what keeps your stomach lining healthy and helps platelets stick together to form clots. When NSAIDs shut down COX-1, your stomach becomes more vulnerable to ulcers, and your blood loses its ability to clot quickly. Put them together? You're hitting the body's clotting system from two sides at once. Your blood can't form clots properly, and your stomach lining is already damaged. The result? Bleeding that starts small-a nosebleed, a bruise, dark stools-and can spiral into internal bleeding you don't even notice until it's too late.It’s Not Just Your Stomach
Most people think NSAIDs and blood thinners only risk stomach bleeding. That’s the myth. The Danish study proved otherwise.- Gastrointestinal bleeding risk: 2.24 times higher
- Intracranial (brain) bleeding: 3.22 times higher
- Pulmonary (lung) bleeding: 1.36 times higher
- Urinary tract bleeding: 1.57 times higher
What About Acetaminophen?
If you’re on a blood thinner and need pain relief, acetaminophen (Tylenol) is the safest choice. It doesn’t affect platelets. It doesn’t damage the stomach lining. It doesn’t interfere with clotting. Yes, it’s not as strong as NSAIDs for inflammation. But for headaches, fever, or mild joint pain? It works. And it doesn’t put you at risk of internal bleeding. The American College of Cardiology and Harvard Medical School both point to acetaminophen as the go-to alternative. No debate. No "maybe." It’s the clear winner.What If You Really Need an NSAID?
Sometimes, you can’t avoid them. Maybe you have severe gout, a flare-up of rheumatoid arthritis, or a sudden injury. In those rare cases, the advice is simple: use the lowest dose for the shortest time possible. Don’t take them daily. Don’t use them for chronic pain. If you need one for a sprained ankle, take it for two days, not two weeks. And never combine multiple NSAIDs. No ibuprofen plus naproxen. No aspirin on top of diclofenac. That’s like pouring gasoline on a fire. Some doctors suggest adding a proton pump inhibitor (PPI) like omeprazole to protect the stomach. But here’s the catch: PPIs don’t stop brain bleeds or lung bleeds. They only help with the stomach. The Danish study showed that even with a PPI, bleeding risk in other organs stayed high. So don’t think a PPI makes it safe. It doesn’t.What About OTC NSAIDs?
This is where things get scary. Most people don’t think of ibuprofen or naproxen as "medications." They’re just painkillers you grab off the shelf. But they’re just as powerful-and just as dangerous-as prescription drugs. In Denmark, most NSAIDs are prescription-only, so researchers could track every single use. In the U.S.? About 30 billion OTC ibuprofen tablets are sold every year. That’s a lot of people unknowingly mixing them with blood thinners. Ask yourself: Have you taken an NSAID in the last month? Even once? If you’re on a blood thinner, you need to tell your doctor. Don’t assume they’ll ask. Most don’t. They’re focused on your heart, your clot, your INR. They won’t think to ask about the Advil you took for your back.
What Should You Do?
- Stop taking NSAIDs if you’re on a blood thinner-unless your doctor specifically says it’s okay.
- Switch to acetaminophen for pain and fever.
- Use heat, ice, stretching, or physical therapy for joint or muscle pain.
- Always tell your doctor or pharmacist about every pill you take-even "over-the-counter" ones.
- Check your medication list every time you refill prescriptions. Ask: "Is this safe with my blood thinner?"
The Bigger Picture
This isn’t just about individual choices. It’s a systemic problem. Doctors don’t always screen for NSAID use. Pharmacies don’t always flag it. Patients don’t realize it’s dangerous. The American College of Cardiology is pushing for electronic health records to automatically warn doctors when a patient on a blood thinner is prescribed an NSAID. That’s the future. But until then, you have to be your own advocate. The bottom line? If you’re on a blood thinner, NSAIDs are not a safe shortcut for pain. They’re a gamble with your life. And the odds are stacked against you.Frequently Asked Questions
Can I take aspirin with a blood thinner?
No. Aspirin is an NSAID and an antiplatelet drug. Even low-dose aspirin (81 mg) increases bleeding risk when taken with anticoagulants. Many people take it for heart protection, but combining it with warfarin or DOACs can double or triple bleeding risk. Always consult your doctor before taking aspirin if you’re on a blood thinner.
Is naproxen worse than ibuprofen with blood thinners?
Yes. Naproxen increases bleeding risk by 4.1 times compared to blood thinners alone, while ibuprofen increases it by 1.79 times. Naproxen is a stronger inhibitor of the COX-1 enzyme, which protects the stomach and helps platelets stick together. That’s why it’s significantly more dangerous.
Can I take NSAIDs if I’m on a DOAC like Eliquis or Xarelto?
No. The risk is the same whether you’re on warfarin, Eliquis, Xarelto, or any other direct oral anticoagulant. The Danish study confirmed this across all anticoagulant classes. DOACs are not safer when mixed with NSAIDs. The interaction is class-wide.
What should I do if I accidentally took an NSAID with my blood thinner?
Stop taking the NSAID immediately. Watch for signs of bleeding: unusual bruising, dark or tarry stools, blood in urine, severe headaches, dizziness, or shortness of breath. If you notice any of these, seek medical help right away. Even one dose can be enough to trigger bleeding, especially in older adults or those with kidney issues.
Are there any natural alternatives to NSAIDs for inflammation?
Yes. Turmeric (curcumin), omega-3 fatty acids (fish oil), and ginger have mild anti-inflammatory effects without affecting blood clotting. They’re not as strong as NSAIDs, but they’re safer when you’re on a blood thinner. Always check with your doctor before starting supplements, as some can still interact with medications.
Sheila Garfield
January 30, 2026 AT 21:06I took ibuprofen for a headache last month and just realized I’m on rivaroxaban. Holy shit. I’m switching to Tylenol today. Thanks for this post-scared the hell out of me in the best way.
Also, why do pharmacies not have warning stickers on NSAID bottles? This should be printed in red on every box.
Shawn Peck
January 31, 2026 AT 19:55THIS IS WHY AMERICA IS DYING. People think OTC means safe. It doesn’t. I saw a guy in the ER last year take two Advil with his blood thinner and bleed out his eyeball. No joke. His wife said he thought it was just for his back. It wasn’t. It was a death sentence with a price tag.
Stop being lazy. Use Tylenol. Or ice. Or cry. But don’t kill yourself over a headache.
Niamh Trihy
February 2, 2026 AT 03:07Great breakdown. The Danish study is one of the most comprehensive on this-I’ve cited it in my pharmacy lectures. What’s rarely mentioned is that the risk starts within 24–48 hours of first use. It’s not cumulative. One pill can be enough, especially in seniors or those with renal issues.
Also, don’t forget that some cold meds and menstrual pain pills contain naproxen or ibuprofen. Always check the ‘Active Ingredients’ label. ‘Pain Relief’ doesn’t mean safe.
Sarah Blevins
February 3, 2026 AT 18:29The data presented is statistically significant, but the causal inference is overstated. The study adjusted for confounders, yet residual confounding from comorbidities (e.g., hypertension, GI pathology) is likely. Additionally, the definition of ‘serious bleeding’ includes minor epistaxis, which may not be clinically relevant.
While caution is warranted, the absolute risk increase remains low for low-dose, short-term use in healthy individuals. The recommendation to eliminate all NSAIDs is overly broad and potentially harmful due to undertreated pain.
Jason Xin
February 4, 2026 AT 10:30Wow. Sarah’s comment is the kind of detached academic nonsense that gets people killed.
I’ve seen patients bleed into their lungs because they thought ‘it’s just a little Advil.’ No one’s arguing about statistical noise here. We’re talking about people who didn’t know. People who trusted the system. The system failed them. And now we’re debating confounders?
Just tell people: Tylenol. Not NSAIDs. End of story. Your ‘nuance’ won’t save a life.
Kimberly Reker
February 6, 2026 AT 06:17My grandma took naproxen for her knees for 10 years and never knew it was dangerous with her blood thinner. She had a brain bleed last winter. We found the bottle in her drawer.
Doctors never asked. Pharmacies never warned. She thought it was like vitamins.
If you’re on a blood thinner, I beg you-go through your medicine cabinet right now. Toss anything with ‘ibuprofen,’ ‘naproxen,’ ‘diclofenac,’ or ‘aspirin.’ Replace it with Tylenol. Even if you think you’re fine. You’re not. This isn’t fearmongering. It’s survival.
And if you’re a caregiver? Do this for your parents. They won’t do it for themselves.
Eliana Botelho
February 6, 2026 AT 17:12Okay but what if you’re allergic to Tylenol? Or have liver disease? Or are diabetic and need something stronger? You just said ‘use Tylenol’ like it’s magic fairy dust.
What about CBD oil? I heard it helps with inflammation. Or maybe I should just suck it up and live with the pain? Or maybe I should stop taking my blood thinner entirely? Because if I can’t take pain meds, why am I even alive?
Also, I read that ginger tea is better than NSAIDs, but I don’t like ginger. What now? Am I just supposed to cry in the corner? This post feels like a guilt trip wrapped in medical jargon. You’re not helping. You’re just making people feel bad for being human.
Rob Webber
February 8, 2026 AT 12:43THIS IS A SCAM. The Danish study was funded by pharmaceutical companies that make Tylenol. They want you to buy their $10 bottle of acetaminophen instead of the $3 ibuprofen. They don’t care about your bleeding. They care about your wallet.
Also, I’ve been taking naproxen with warfarin for 8 years. I’m fine. My INR is perfect. You’re all panicking over nothing.
Stop fearmongering. Trust your body. Not some study from a country that doesn’t even have decent coffee.
Adarsh Uttral
February 9, 2026 AT 01:24bro i took ibuprofen for my back last week and i’m on xarelto… i’m gonna go check my stool now lmao
also why do all these articles sound like they’re written by a doctor who hates people? just say ‘don’t do it’ not ‘the COX-1 enzyme pathway is compromised’
Yanaton Whittaker
February 10, 2026 AT 13:36Only in America do people die because they took a painkiller. In Russia, we just take vodka and pray. No study needed.
Also, this post is weak. Real men don’t use Tylenol. We use aspirin, naproxen, and a shot of whiskey. If you bleed, you bled too slow. That’s just life.